April 24, 2013
I am writing to let you know that Charlotte passed away on April 24, 2013. She died as she had lived in peace and with concern for others. A Celebration of her life will take place at her much loved Julian Library on May 26th at 2:00p.m. In lieu of flowers, those who wish may make a donation to the Friends of the Julian Library in her name (The Friends of the Julian Library: P.O. Box 815, Julian CA 92036. Please note that your gift is made in the name of Charlotte Mitchell). Anyone wishing to assist with the coming celebration, may contact Mary Morgan at maryfmorgan@gmail.com
The Mitchells are not active in social media but Brent would be grateful if those of you who are, would use it to alert others that you know who would want to know of her passing.
Brent also wants you to know that he will be writing a final post but asked me to send this one.
Mary Morgan
March 15, 2013
Charlotte had her Avastin today. The Avastin dosage has been increased from 2mg/kg to 4mg/kg, and the CPT-11 has been discontinued. Her newest clinical symptom is dysphagia (difficulty swallowing), which has put a stop to most of her medications in pill form. Two weeks ago at Avastin she weighed 132 lbs, and today she weighed 124 lbs. Statistics vary, but about 50% of people with cancer die from cachexia and not from the cancer. Nothing seems to even stabilize her cachexia, and her other clinical symptoms continue to increase.
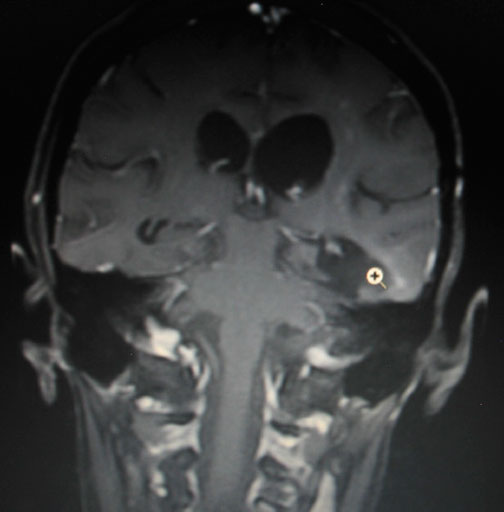
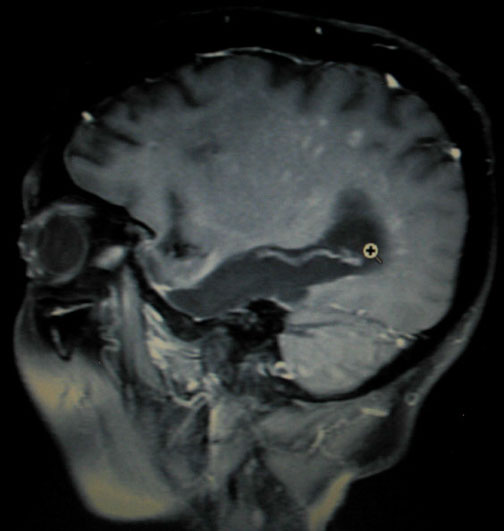
Her MRI on March 7th was read as stable.
"...The current examination fails to demonstrate evidence for residual, recurrent, or mobilizing tumor...."
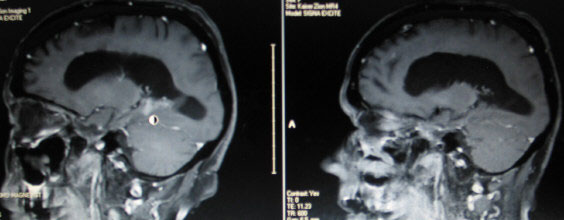
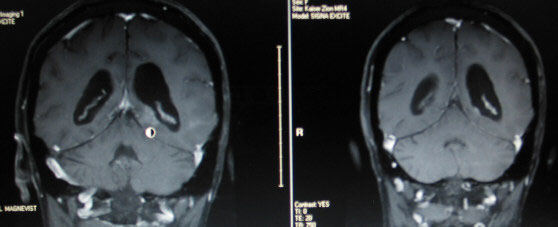
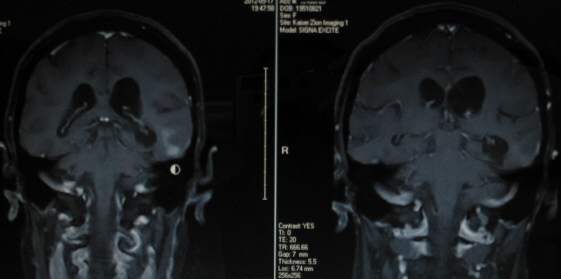
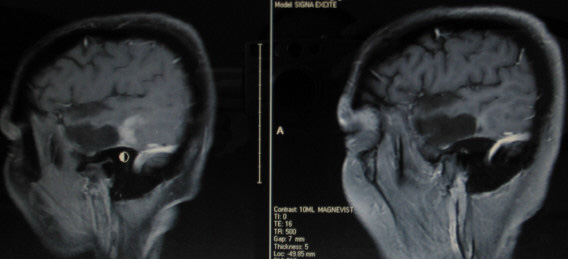
The neuroradiologist did not comment on the following specific views that seem to show possible new infiltrative tumor.
The cursor in the first COR-POST image is located in the original resected tumor bed. You can see just to the right of the cursor a curvilinear pattern of white enhancing spots rising upward and around the ventricle. The initial white enhancement bordering the cavity is old tumor gliosis. Rising above the gliosis are the new spotty areas of concern.
Just to the right of the cursor in the below SAG-POST image you can see another curvilinear pattern of scattered white enhancing spots again rising upward and to the left, and then downward.
This disease increasingly wants to demean and degrade its victims. However, as she continues to decline, Charlotte faces each new day with her usual grace and dignity.

March 1, 2013
Charlotte had her low dose Avastin (2mg/kg) this morning. The CPT-11 was held. She continues with her Temodar at 40mg 2X daily, along with her Metformin at 500mg 2X daily. The Metformin was restarted in January, but the Celebrex continues to be held. Since our last update, she has received her Avastin and CPT-11 every two weeks. The CPT-11 was initially dosed at 60mg/kg, but was reduced to 40mg/kg on 1-18-2013.
Charlotte is facing many challenges. Foremost is her cachexia. She has lost 20 pounds (151 lbs to 131 lbs) since starting CPT-11 on 12-07-2012, and the muscle wasting has been horrific. Her other clinical symptoms have continued to increase. Today she can no longer walk, speak, read or write. She has also lost the use of her right arm and hand. She is so weak that she is unable to even move her body in bed.
Her next MRI is this Thursday, March 7th.
Her last MRI on 1-10-2013 showed continued shrinkage in her 5-17-2013 tumor and her 11-29-2013 tumor.
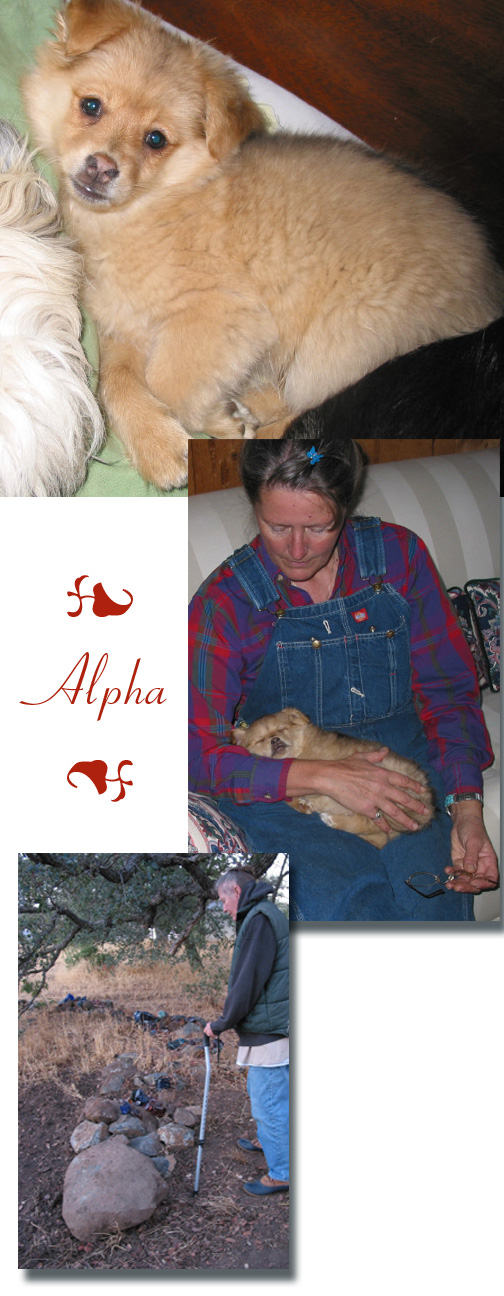
Below is our newest rescue. Snuggles is a poodle/terrier mix. The picture was taken about a month ago at 8 weeks of age.

December 7, 2012
Charlotte has had her Avastin (2mg/kg) every two weeks along with her daily Temodar (40mg 2X daily) since our last update. Her metformin and celebrex continued to be held due to her kidneys.
She had her MRI on Nov 29, 2012. It showed another recurrence.
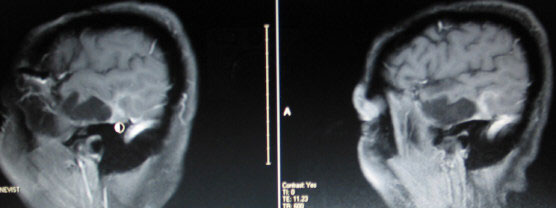
Below are images from her Nov 29th MRI on the left and her Oct 4th MRI on the right. The tumor is the white enhancement directly above the round cursor.
My measurements show it to be 2.4 cm X 1 cm.
Below are images of her May 17th recurrence.
Again, the left image is from the Nov 29th MRI and the right image is from the Oct 4th MRI.
Her new treatment plan includes keeping the Avastin (2mg/kg) and her metronomic Temodar (40mg 2X daily). She now receives CPT-11 (65mg/m2) every two weeks along with her Avastin. Her metformin (500mg 2X daily) has been restarted. The celebrex continues to be held.
While sitting in the chemo room today while Charlotte received her CPT-11 and Avastin, I received the written MRI report.
It states:
1. "Persistent stable extensive posttreatment changes to the brain.... These changes appear overall stable as compared to prior recent MRI scans."
2. "With the administration of gadolinium previously documented and described "wispy" enhancement involving the dorsal surface of the postsurgical cavity appears if anything slightly improved in the interval, less nodular, and exhibits less enhancement character than previous studies. There are no new areas of abnormal enhancement character involving the remainder of the brain elsewhere to suggest mobilizing tumor."
The neuroradiologist missed the new tumor.

October 26, 2012
Charlotte had her low dose Avastin today and every two weeks since our last update. She continues with her metronomic Temodar (40mg 2X daily). The metformin and celebrex continue to be held until her labs show improvement in her proteinuria.
Since our last update, Charlotte's
1. sodium is in the low end of the normal range,
2. weight loss has stabilized and her muscle wasting syndrome (cachexia) has shown improvement,
3. hypertension has also improved.
She now presents with:
1. a UPC ratio near 2.0,
2. occasional double vision,
3. slight numbness on the right side of her face,
4. her usual neuropathy in her legs and right hand.
Her October 4th MRI stated:
1. "Over the series of examinations there continues to be decreasing enhancement in the left temporal lobe....
Although enhancement is still present it is becoming more linear and less nodular over time especially as
compared to May 2012 study."
2. "Several small foci of increased T2 signal intensity on the brainstem are also stable."
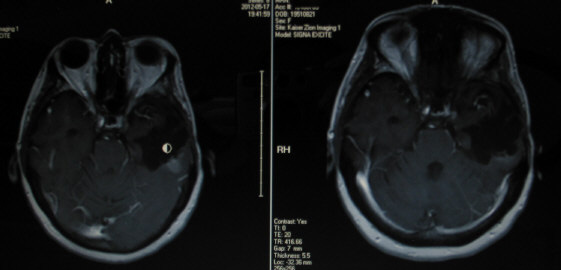
Below are images from her 10/4/2012 MRI (left) and 5/13/2012 MRI (right).
Tumor is the white enhancement located above the round cursor in image 1,
and to the left of the round cursor in image 2.
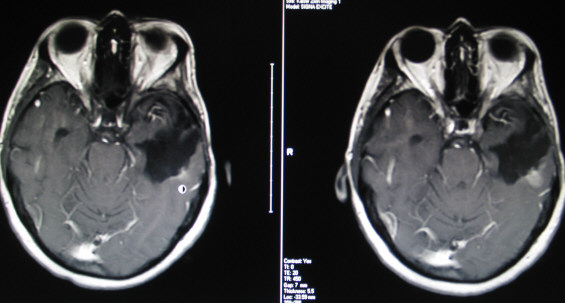 image 1 image 1
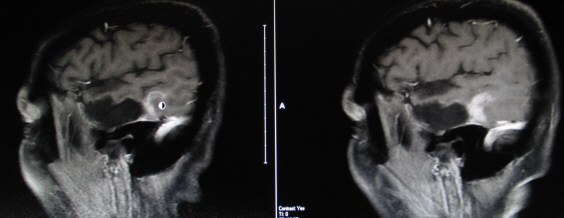 image 2 image 2

August 31, 2012
Charlotte had her Avastin (2.0mg/kg) on August 17th and again today. She continues her metronomic Temodar (40mg 2X daily). The metformin and celebrex have been held because of her kidneys. She presents with: hyponatremia (low sodium), cancer cachexia (lost 5% of her body weight in 3 months), hypertension (blood pressure not controlled by medication), UPC (urine protein-creatinine) ratio above 2.0, nausea with vomiting, and increased neuropathy (which makes walking very difficult).
Her August 9th MRI stated:
1. "Since 5/17/12 there has been interval decrease in size of a zone of nodular enhancement.... Central non-enhancement/necrosis has appeared in the lesion. These findings suggest improvement in recurrent tumor.
2. There remains slight blurring of the signal intensity difference between white and gray matter on T2 and FLAIR images within much of the left temporal lobe... I cannot exclude the possibility of nonenhancing tumor infiltration throughout much of the left temporal lobe.
3. Abnormal results clerk informed."
Below are images from her 5/13/12 (left) and 8/9/12 (right) MRI.
Tumor is the white enhancement located above the round cursor.
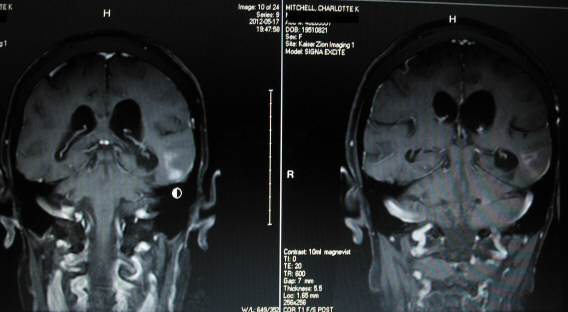
image 1
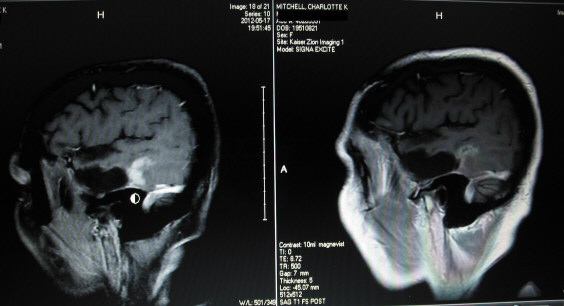
image 2

RIP: Sophie Mitchell
August 3, 2012
Charlotte had her low-dose Avastin (2.0 mg/kg) this morning. She has had her Avastin every two weeks since our last update, along with her daily Temodar, celebrex and metformin.
Her MRI on June 21st read as follows:
"Unfortunately, over the last two studies there is a pattern of progressive nodular enhancement and greater conspicuity with gray-white blunting of the left temporal deep... This focus of nodular enhancement has increased to measure 16 X 11 X 20mm versus 15 X 10 X 17mm...."
Due to the increased growth in the enhancing tumor, we increased the Temodar to 40mg 2X daily on July 10th.
There is no treatment for the non-enhancing tumor.
She has basically lost her speaking, writing and reading abilities. Thankfully, her ability to work and create new sculptures has never been affected. Her next MRI is Thursday, August 9th.

June 8, 2012
Charlotte had her low-dose Avastin (2.0mg/kg) this morning and continues her low-dose Temodar (20mg 2X daily).
We attended the artist reception at the Del Mar Fair last night. After her Avastin this morning, we returned to the fair for an enjoyable day. She always loves it because it is the one day of the year that she deviates from her strict diet.



May 25, 2012
Since our last update, Charlotte had her Avastin (1.75mg/kg) on April 27th and May 11th.
Charlotte's May 17th MRI was read as abnormal. It showed both enhancing and nonenhancing tumor growth. Clinically, she presents with severe expressive aphasia. She knows in her mind what she wants to say but is unable to verbalize her thoughts.
Her new treatment plan includes Avastin (today's dose increased back to 2.0mg/kg) with metronomic temodar (20mg orally 2 times daily), along with celebrex (100mg 2 times daily) and metformin (500mg 2 times daily).
Below are images from Charlotte's current May 17 2012 MRI (left side) and her previous Mar 22 2012 MRI (right side).
Left image below shows tumor (white enhancement below the circular mouse cursor) in AX T1 POST.
Left image below shows tumor (white enhancement above the circular mouse cursor) in COR T1 POST.
Left image below shows tumor (white enhancement above the circular mouse cursor) in SAG T1 POST.
The tumor measures 2.2 cm SI by 1.5 cm ML by 1.3 cm AP.
Research shows:
"A nonenhancing tumor pattern of progression is common after treatment with bevacizumab (Avastin) for GBM and is correlated with worse survival."
"Treatments after bevacizumab (Avastin) failure provide only transient tumor control."
Charlotte's next MRI will be June 21st.


April 13, 2012
Charlotte had her low-dose Avastin (1.75mg/kg) today. Since the last update, she also had her Avastin on March 16th and 30th, and on April 13th and 27th. She still presents with aphasia and neuropathy, but these both significantly increased shortly after the last update. Charlotte also had her regularly scheduled MRI on March 22nd, which was read as stable.
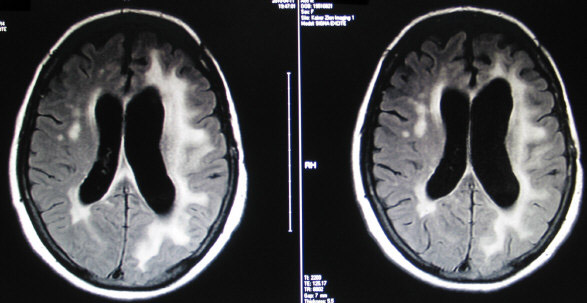
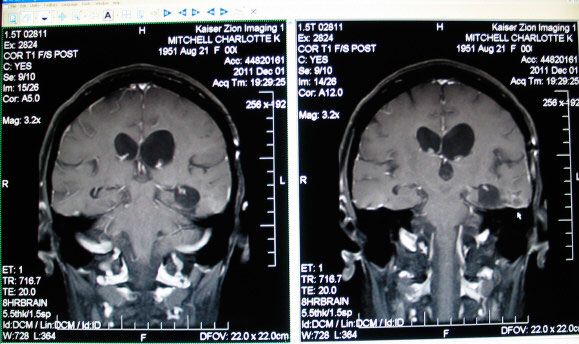
Below are T2-FLAIR images of her leukoencephalopathy. The left image dated JAN 2008 was after her surgery but before her radiation and Temodar with Avastin. The right image dated DEC 2008 shows the effects consistent with late stage radiation damage.
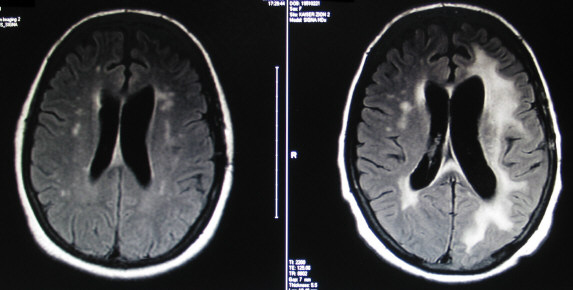
The left image below, dated APR 2010, shows the leukoencephalopathy when she commenced her current low-dose Avastin. The right image is dated MAR 2012. The leukoencephalopathy has basically been stable since DEC 2008.
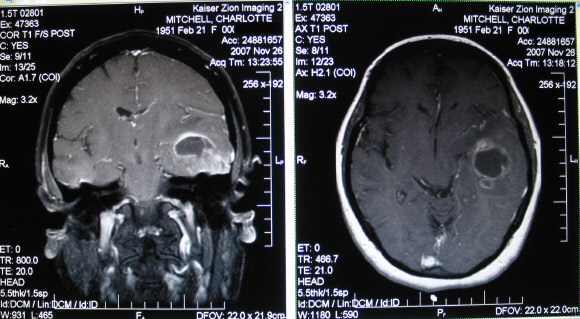
The following images, dated Nov 26, 2007, show Charlotte's glioblastoma multiforme and edema before her Dec 4th surgery.

February 3, 2012
Charlotte had her low-dose Avastin(1.75mg/kg) this morning.
Below are two images from Charlotte's MRI on Mar 14 2010 when she started Avastin at 2mg/kg for her glioblastoma recurrence.
The two consecutive post-contrast "slices" show enchephalomalacia/gliosis (softening of the brain/scar tissue). These enhanced areas are located on the floor of the resected tumor bed. The recurrent tumor is barely visible, but is greatly enhanced in 7 other "slices", all marginating the left ventricle. The ventricles are the two "elliptical" dark areas in the center of the brain. (The left ventricle is on the right side in the image.)
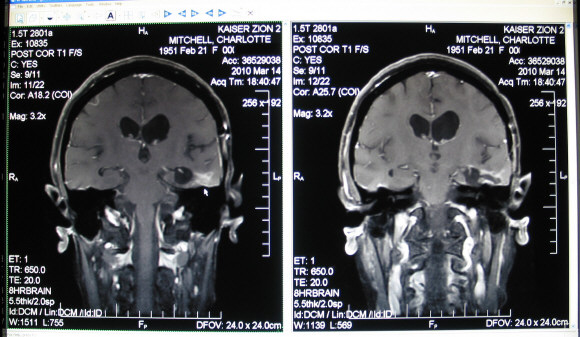
Below is the last MRI (Dec 2 2011) before the Avastin dosage was lowered from 2.0 to 1.75 mg/kg.
Every MRI after Mar 14 2010 showed a continuing decrease in tumor enhancement until Dec 1 2010, when the nodules became almost invisible. The enchephalomalacia/gliosis continued to show a continuing decrease in enhancement through her Dec 1 2011 MRI. Radiologically, Avastin has been a miracle drug.
One side effect of radiation therapy and chemotherapy is brain atrophy. On the MRI this can be seen in the increased size of the black areas representing cerebrospinal fluid.
Charlotte's Jan 26 2012 MRI was read as stable. Some enhancement occurred in the Dec 1 2011 right photo above, representing the first reversal in 22 months of decreasing enhancement. It was not mentioned in the written MRI report, but is nonetheless concerning. We will continue with the lower Avastin dosage of 1.75mg/kg.

January 20, 2012
Charlotte had her low-dose Avastin(1.75mg/kg) this morning.
In the last update, I outlined her Avastin treatments. Today I will explain more about her Temodar treatments.
As a preface, the following is obviously not recommended for others, especially without the consent of their doctor.
These were personal decisions that Charlotte and I made together in order to add some quality of life to her remaining time. We kept these decisions private only as "a path of least resistance". It is disclosed now in hopes of adding to the GBM knowledge base. Maybe it will somehow aid others, since there are no winners in this fight. Just those that seem to be a little luckier.
After her radiation and concurrent Temodar(75mg/meter squared) treatments, Charlotte began her monthly Temodar(5/23 schedule at a dose of 150mg/m2) on Feb 28 2008. She concurrently took Avastin(10mg/kg) every two weeks. The UCLA/Kaiser study called for an increase in the Temodar dose to 200mg/m2 in cycle 2 if the patient had no adverse reactions to cycle 1.
Charlotte could not handle the higher dose of 200mg/m2. She had a platelet transfusion, Neupogen shots for low WBC, missed chemo appointments (low ANC for Avastin and low platelets for Temodar), ER visits, along with numerous other side effects. She went back to 150mg/m2 dose of Temodar starting with round 3.
I researched the earlier clinical study of 10 patients that preceded her study. At the time of publication, five of the ten patients were receiving Temodar at 150-200mg/m2. One patient had died. However, four of the ten patients were receiving Temodar at <150mg/m2. Certainly no cause and effect, but the patients taking <150mg/m2 were still alive.
After many serious talks with Charlotte, I lowered her nightly Temodar dose starting with cycle 7 on Sept 4 2008.
(Exact cycle and date needs to be verified by my other paperwork.)
She still received all of her prescribed 100mg Temodar pills, except for taking 3X100mg pills for 5 nights, she started with 3X100mg pills the first night, but received 2X100mg pills for nights 2-7. The fifteen pills were now spread out over 7 nights. You could say her new Temodar dose was now 7/23(100mg/m2). It began as a trial dosage in the beginning, but with a few exceptions, became the norm over the next 17 months.
I also dramatically increased her supplements and tried a few off-label drugs. Her CBC counts and energy returned.
Her MRIs continued to be "stable", but there continued to be very subtle encephalmalacia/gliosis rim-enhancement in her tumor bed.
On Charlotte's Oct 26, Nov 24, 2009, and Jan 22, Feb 19, 2010, MRI's, they were read as "stable" but the neuroradiologist noted a "nodular process marginating the post surgical cavity... becoming more prominent compared to prior studies".
On Feb 25 2010, after 25 Temodar treatments, Charlotte stopped all chemo. The standard neuro-oncology procedure was to stop Temodar after 24 cycles.
Her Mar 4 2010 MRI showed "definite and unequivocal multifocal regions of abnormal enhancement". We tried Temodar(5/23) again for one month.
Her Apr 11 2010 MRI showed "mild progression in size and number of the enhancing nodules...compatible with metastases from glioblastoma multiforme".
Charlotte's third try with Avastin started on Apr 16 2010. She was also prescribed concurrent Etoposide, which I never gave her. Research showed a Duke study finding the combination of Avastin and Etoposide no more effective than Avastin monotherapy for recurrent GBM. Also, Charlotte's second try with Avastin lasted only four treatments because of her kidneys. Etoposide can also cause renal dysfunction. The last thing I wanted to hear four treatments later was that Avastin was controlling the tumor, but her kidneys will not allow further treatments.
We have been very, very lucky. Her next MRI is Thursday, Jan 26th, and we will hopefully see Zari.

January 6, 2012
Charlotte had her low-dose Avastin today. She still presents with increasing expressive aphasia and peripheral neuropathy. The following is a brief history of Charlotte's Avastin treatments, and how we ended up on the current Avastin dosage.
Charlotte had GBM surgery (partial resection; tumor 5.5 cm) on Dec 4, 2007. She enrolled in the UCLA/Kaiser study for newly diagnosed GBM patients using Avastin/Temodar. She started Avastin on Jan 3, 2008 at 10mg/kg every two weeks. Her last Avastin treatment on study was Apr 2, 2009 due to her high UPC ratio. I had permission from UCLA (Dr Cloughesy) to reduce the Avastin to 5mg/kg if and when Charlotte's UPC ratio returned to within trial limits (UPC<1). It never did, and she was dropped from the study on June 30, 2009.
Her second try with Avastin was on Oct 22, 2009 at 5mg/kg. The 5mg/kg lasted only two treatments, before her UPC ratio climbed dramatically. We lowered her Avastin to 2.5mg/kg for the next two treatments. Because of continued high UPC ratios, she went off Avastin on Nov 19, 2009, after a total of only four treatments.
From Feb 28, 2008 thru Mar 17, 2010, she also received 26 Temodar treatments.
Her Apr 11, 2010 MRI showed multifocal "abnormal enhancement consistent with tumor recurrence" gave Charlotte her third try on Avastin. On Apr 16, 2010, she started her 2.0mg/kg dose as a monotherapy. She has received that dosage every two weeks. On Dec 23, 2011, we reduced the dose from 2.0 to 1.75 mg/kg. We hope to still "control" the tumor but alleviate some of her progressing clinical symptoms.

December 23, 2011
Charlotte had her newer low-dose Avastin (1.75mg/kg) this morning.
Three more good articles relating to chemo and radiation induced neurocognitive problems are:
1) Neurocognitive Complications of Cancer Therapy
2) Neurologic Complications of Cancer Therapies
3) Phase II Study of Donepezil in Irradiated Brain Tumor Patients: Effects on Cognitive Function, Mood, and Quality of Life
Zari and Nasser Pirasteh are pictured below with Charlotte. The sculptures in the background are just an example of those that reside on the inside and outside of Nasser's biggest sculpture; their home. There was an instant bond between Zari and Charlotte while Zari was doing Charlotte's MRIs over the past few months. Zari invited us to dinner last Thursday to meet her husband, her son and his wife. We had the most enjoyable evening talking about art, philosophy, poetry, Rumi, life....
Thank you Zari for inviting Charlotte to your home, and into your heart.

December 12, 2011
My computer had a hard drive failure, so please excuse my tardiness.
Charlotte had her low-dose Avastin (2mg/kg) on Nov 25th and Dec 9th. She had a brain MRI on Dec 1st and we met with her NO this morning. Her MRI was read as stable.
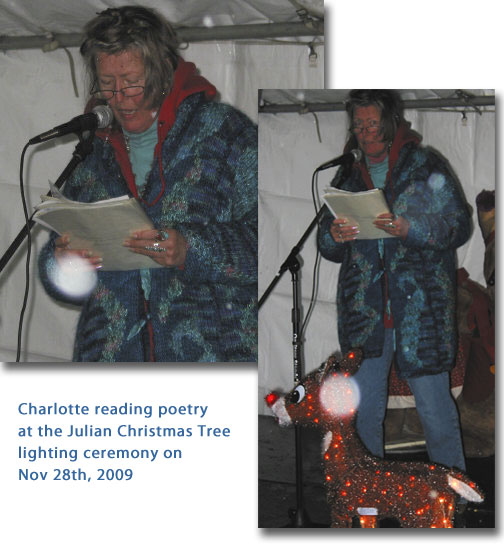
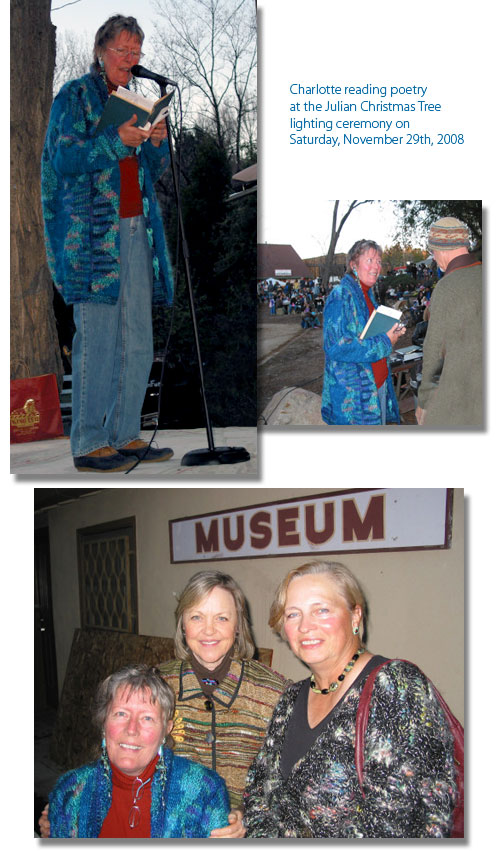
Charlotte and our pet Cyrus celebrated her four year anniversary by reading poetry with "Pets and Christmas" themes at the Julian Christmas Tree Lighting Ceremony on Nov 26th. Her aphasia and neuropathy have increased dramatically, but the pathway in her brain for reading the written word seems unaffected.
Charlotte is suffering from radiochemotherapy-induced leukoencephalopathy. An excellent article in The Oncologist is "Clinical Patterns and Biological Correlates of Cognitive Dysfunction Associated with Cancer Therapy"
.full is a must read for anyone with glioblastoma and its associated neurocognitive impairments. Table 1 is especially informative. Another excellent article is "Neurologic Complications of Chemotherapy".
I would like to share the following two eulogies. The first is written by Wall Street Journal reporter Bret Stephens. The second is written by my friend Shelly, mentioned in the June 10, 2011 update.
Bret writes:
Does the manner of our dying count in the final reckoning of how we have lived our lives? Nearly my first assignment at the University of Chicago was to read the Platonic dialogues on the trial and death of Socrates. "Then, holding the cup to his lips, quite readily and cheerfully he drank off the poison." It is the supreme moment in the Western philosophical tradition, when wisdom and courage, resignation and defiance, combine to overcome injustice and, in a sense, death itself.
Would that we could all die as Socrates did. Generally we don't. "The good death has increasingly become a myth," wrote the Yale surgeon and bioethicist Sherwin Nuland in his 1993 prize-winning book "How We Die." Dying, in Dr. Nuland's eloquent telling, amounts to "a series of destructive events that involve by their very nature the disintegration of the dying person's humanity." Who can—who would dare—judge a man's worth when his mind and body are being picked bare
by disease?
I've been thinking about all this for over a year now as I watched a brain tumor, along with the associated medical interventions, pick away at my father bit by bit. First, an operation to remove the tumor, which erased his right field of vision and took away his ability to read and drive. Next came debilitating bouts of chemo and radiation, along with an agonizing case of shingles. Then avascular necrosis set in, leaving him unable to walk. Later, as the tumor returned, his
memory began to slip. Near the end he was almost totally blind, couldn't utter a sentence, couldn't swallow a pill, couldn't hold his food down. Cancer is a heist culminating in murder....
Shelley writes:
Dear Brent and Charlotte,
My sweet big sister Pam, died last night, on her 63rd birthday. She had been resting comfortably in bed since the day after Thanksgiving. Pam was ready for God to take her Home with him and we are rejoicing that she didn't have any pain and her death was a wonderful transition into Heaven. It has been such an honor to be Pam's sister and to have been able to spend a good amount of time with her over the last almost 8 months.
Glioblastoma is a horrible disease. Pam taught me a lot over this time, and although her cognitive skills were affected pretty dramatically right after the diagnosis, she fought as much as she could to try to regain or at least retain as much as possible by all the various drugs, supplements, reading and trying to master puzzles. She didn't ever really give up. But when that last MRI showed growth and she started suffering more seizures which then would affect something else, Pam was ready to rest and let God take over completely.
I think and pray for you both daily. I haven't heard from you in awhile and hope Charlotte is comfortable and still able to sculpt.
We will take one day at a time and celebrate Pam's life and the wonderful memories she made for us.
Sincerely,
Shelley

November 11, 2011
Charlotte had her low-dose Avastin (2mg/kg) today. Since her last Avastin treatment two weeks ago, I feel Charlotte's aphasia and neuropathy has increased at a faster rate.
I ran across the following postings on a brain tumor site while doing some technical research.
The first is a summary of postings by Craig's wife Barbara and the latter is one of Barbara's last postings.
Charlotte has most of Craig's subclinical symptoms mentioned in the first five lines. I agree with Barbara that everyone on or contemplating the use of Avastin should be aware of these possible side effects.
- Craig was on Avastin form Sept '07 until September '09 and he had all sorts of damage from the Avastin to his vascular system, especially to the vascular nerves.
- had severe neurodegeneration.
- ended up practically paralyzed on is right side with terrible pain
- he could no longer work, he could no longer walk without assistance and was having major speech problems.
- Craig had 2 recurrences in the 3 years- when it was recurrence in mass form it was easier to get a handle on-
when it was diffuse it insidiously spread while on Avastin even though the scans looked pretty excellent.
- by the way the tumor became diffuse at the 18th month on Avastin.
- Sure enough it came back showing Avastin was 100% the cause of the kidney failure.....even though the urine tests always came back OK.
- I just want people to know what they up against when dealing with Avastin
Love, Barbara
Jan 4, 2010
Last evening at 7:30 my beloved Craig died of his brain tumor. He was in my arms and surrounded by our family an a friends, but it was a very physically hard death that took 3 days of intensive agony on his and my part, after several months of terrible deterioration first losing his ability to walk and use his right arm, losing almost all speech except a couple of words, and then losing most of his sight.
Many gathered to be with him while he was dying- give their love and support him. Craig had a ravaging brain tumor but his body was still young and strong. He did not have the kind of death where you die peacefully sleeping.
He died very hard, choking and gasping for 2 nights and two days. The only solace is that we were able to hold him and also to fulfill his wishes for his last moments and he is at peace now with no more pain or agony. He was extremely brave and said this dying of the brain tumor once we let nature take it's course was the hardest thing he had ever done. He wanted to die with grace and with dignity, an example of how to live rather than how to die, and he did just that.
He lived just about exactly 3 years with his gbm.
Love, Barbara
Never Give in, Never Surrender, and NEVER Ever, EVER Give up HOPE!... Mike Gabriel's (RIP) tag line.

October 28, 2011
Charlotte had her low-dose Avastin today. I have continued the addition of some salt capsules during the past two weeks. Her serum sodium was at 138 again (normal 135-145). She still presents with increasing aphasia and neuropathy.
Tribute to Snoogie.
Every once in a while, if you are fortunate, one is blessed with a special friend that somehow touches your life. This friend was a beautiful White Shepherd dog. She brought us sincere joy and friendship. After a week of house sitting, I vividly remember how my eyes swelled up as she and her sister continued staring at me as they departed in their mother's camper shell.
Snoogie: Requiescat in pace et in amore. You will forever live in our hearts.

October 17, 2011
Charlotte had her low-dose Avastin last Friday and we met with her NO today. Her labs last Thursday showed her serum sodium was finally in the normal range. I had to give Charlotte an extra five grams of salt each day to raise her sodium level. We see her nephrologist this Thursday, so I will advise her that her "no salt diet" has to be changed.
Charlotte's MRI on October 6th was stable.
Don't ask me why, but I kept coming back to the following two posts and felt that I needed to post them.
They are extraordinarily powerful and thought provoking.
Death with dignity
My wife Meg died on Saturday morning in the loving company of her brother, sister, son, daughter and husband.
Suffering from a disease that robs one of intellect and dignity, she had the option, as a Washington resident, to choose the time of her death. She used the provisions of Washington's "Death with Dignity" Act to hasten her death, while
she was still able to converse with and understand her family members. (Oregon has long had a very similar "Aid in Dying" act, Vermont is considering one. link.
Her family gathered on Friday and spent the day with her. She was much more alert and animated than of late and visited with each of us. Despite knowing that her death was the next day, we all slept well that night (I slept much
better than for many weeks), showing us that we were prepared for her passing.
Social workers (she met privately with one from hospice and one from Swedish Hospital to affirm her decision) and the volunteer from "Compassion and Choices Washington" all remarked on her readiness (and that how she had not been ready the previous week).
The volunteer from "Compassion and Choices Washington" showed immense skill and empathy in helping Meg and in caring for us.
Meg died peacefully and quickly, with no signs of discomfort. It was a remarkable end to a long struggle, and released Meg from what we all knew could be a long, distressing, undignified and inevitable end.
Our preparations, the company of relatives, Meg's peaceful passing and the knowledge of her command of the situation all served to make her passing much easier for us all.
Thank you all for your advice and encouragement over these last almost two years.
Andrew
Husband of Meg GBM dx 12/09
95% resection 12/09; radiation
RTOG 0825 trial 1/10 - 2/2/11:
Temodar + Avastin (now unblinded)
Progression at original site 3/4/11, uncal seizures
Wada test on 3/18/11
Awake craniotomy 3/22/11 removed all enhancing material
Unhealed incision revised by neurosurgeon, 4/25/11
MRI, 4/28/11: progression, enhancing and non-enhancing, restart Temodar
Second incision revision, plastic surgeon, 5/10/11
MRI, 5/18/11: further progression.
Restart Avastin 5/19/11, some effect
MRI 6/24/11: tumor growth despite Avastin
8/2/11: Avastin
8/8/11: start hospice - staying comfortably at home with help from Meg's
brother
10/1/11 death (with dignity)
______________________________________________________________________________________________
Death with Dignity HBO movie available for on demand viewing
You may recall that my wife recently used our state's Death with Dignity law to end her journey with glioblastoma, in the company of her loving family. link
Last night I attended a showing of an HBO movie about Death with Dignity, entitled "How to die in Oregon"
It's available for on demand viewing on HBO from today through November 13th:
It's a difficult movie to watch, particularly if you have just lost a love one (though I found the experience therapeutic) but I wanted to bring it to your attention.
While most of the discussion here is rightly about live-prolonging treatments, I think we all know (from the condolences expressed here) that for most patients the end is inevitable.
I commend this movie to you as a sensitive exploration of a final treatment option for your loved ones that is available in a few US States.
It may well not fit in with your beliefs or ethics, but it was my wife's freely chosen wish and I had the honor as her husband to help her fulfill it.
Andrew

September 30, 2011
Charlotte had her low-dose Avastin today. Her labs yesterday showed her serum sodium had fallen from 133 to 130.
Her aphasia is about the same as two weeks ago, but at times she is beginning to show a little frustration. In her mind, Charlotte knows the word(s) she wants to say, but somehow that pathway of verbalizing her thoughts is affected.
Last update I wrote about her radiation and chemotherapy treatments, along with the tumor location, as being the probable causes of her aphasia and neuropathy. It could also be recurrent tumor.
Charlotte's next brain MRI is this Thursday, October 6th.

September 16, 2011
Charlotte had her low-dose Avastin today. Her labs yesterday showed her serum sodium had risen from 126 to 133 (normal 135-145). Her speech was initially slightly improving, but it did not keep pace with the rise in her sodium level.
Charlotte seems to be in good health, as shown by her labs and her appearance. However, her kidneys and blood pressure are still the weak link in her labs.
"Tumor control" will always be our number one concern, but her aphasia and neuropathy have never "stabilized" over these 45 months. They both gradually keep getting worse. I associate this continued decline to her earlier radiation and chemotherapy treatments, along with her initial brain tumor location. All of her supplements, off-label drugs and diet have been directed at "controlling" her tumor and improving her immune system and overall health. I will now be dropping most of her supplements for her general health, and adding some that may help to "stabilize" her neuropathy and aphasia.

September 5, 2011
Charlotte had her low-dose Avastin (2mg/kg) last Friday. On Thursday she had increased difficulty with her speech, and she told me that she thought her serum sodium was low again. Her labs later that day showed her sodium was 126 (normal 135-145). She had been on a high dose supplement the previous three days that can also act as a diuretic. I stopped the supplement and slowly increased her salt intake. Her speech has been steadily improving.

August 22, 2011
Charlotte had her Avastin on Friday, and we met with her neuro-oncologist today. Her last MRI came back "stable". Her last labs showed her serum sodium had fallen again from 132 to 131.
I have added the following supplements to Charlotte's list: huperzine A, vinpocetine, phosphatidylcholine, L-carnosine and bacopa monniera. I have increased her dosage of R-lipoic acid bio-curcumin, omega-3, resveratrol and sulforaphane.

August 5, 2011
Charlotte had her Avastin this morning. Here are some more lab results:
TOTAL CHOLESTEROL result 108 standard range <200
LDL CHOLESTEROL result 50 standard range <100
HDL CHOLESTEROL result 49 standard range >/=40
TSH (Thyroid Stimulating Hormone) result 2.89 standard range 0.35 - 4.00
GLUCOSE, RANDOM result 97 standard range 70 - 140
Her serum sodium level has risen from 129 to 132 over the past two weeks, but is still below the 135 target level.
Perhaps related, there has been the return of some occasional slurred words in her speech. That is how this all began in Nov 2007.
Her next brain MRI is this Thursday, Aug 11th.

July 25, 2011
Charlotte had her Avastin last Friday. Her labs from the previous day showed she had a serum sodium level of 129. Normal is 135 -145. Anything below 135 is called hyponatremia, which Charlotte occasionally has because her kidneys have a problem holding sodium. As long as her level is above 130 she seems fine. Anything below 130 causes her to have more problems with her speech. She increased her salt intake over the weekend and her speech has returned to where it was about a week ago.
A few other lab results that some might find interesting were:
CALCIUM result 9.5 normal 8.5 - 10.7
VITAMIN D, 25-HYDROXY result 140 normal 30 - 100
HGBA1C (blood sugar) result 5.6 normal 4.8 - 5.9
LEAD, BLOOD result <2 normal <10
C-REACTIVE PROTEIN result <5 normal <10
The Vitamin D3 result is high, but it is where I want it for Charlotte as along as her calcium level is normal. This is the first time the C-reactive protein test was done, and I wish I had a baseline result from Dec 2007 for comparison. I do not know if brain tumor patients show an elevated result, and if so, how elevated. Further research is needed.

July 8, 2011
Charlotte had her Avastin this morning. Her aphasia and the neuropathy in her extremities continues to gradually increase.
A valuable website that I use is Pill Advised
- Know What You're Taking.
Login and enter all of your medications, both prescription and/or supplements. It will inform you about both good and bad interactions, along with "possible interactions". "Helpful supplements" is another useful category.

June 27, 2011
Charlotte had her Avastin last Friday, and met with her neuro-oncologist this morning. Her June 16th MRI was stable.
Her clinical symptoms of aphasia and numbness continue to increase. This written MRI used the words "ischemic change", "senescent change" and "global atrophy". This damage can be caused by chemo, radiation, high blood pressure, etc. The MRI T2 and T2 FLAIR views show these very slow growing changes. This written MRI also noted presumed post radiation damage to the bone marrow in the upper neck and skull base structures.
I remember reading in an interview with a doctor a few years ago who stated "Avastin does work like a miracle drug for a few patients...". So far, Charlotte is one of those patients, especially at the dosage of 2mg/kg. Her recurrence appeared on her March 2010 MRI. There were at least six new tumor sites located away from the original tumor cavity. Most were located deep in her brain marginating her left ventrical. All of her MRIs until Dec 2010 showed continued tumor shrinkage. Some neoplasms even disappeared. Since Dec 2010 the MRIs have shown no changes in the remaining tumor sites. The blood vessels in these sites are still leaky though, because if the MRI technician is slow when doing the post contrast series, more contrast will leak out and the written MRI will report "possible enhancement" as was reported in her Feb 2011 MRI. As I mentioned in an earlier update, the AX T1 POST view was replaced by the COR T1 POST and the DWI views as the first ones that I read on my disc copy.
I have also made the following changes:
- On MRI dates, I have been adding and/or rotating some supplements for the two months until the next MRI. This will hopefully give me a better idea of what might be working to help control the tumor.
- I now give Charlotte lean red meat. For the first three years, she ate only salmon for lunch. Six months ago I changed from salmon to chicken.
- I have changed to liquid extracts whenever possible. It is only about 5% of Charlotte's supplements, but it does help with pill fatigue.
- Because of the summer heat, I have reduced her walks and changed to isometric exercises and tractor rides. I set up an "obstacle course" that she and Cyrus drive through for 20 minutes two times a day.

June 10, 2011
Charlotte had her Avastin this morning, and then we had a fun time at the Del Mar Fair. We also attended the artist reception last night. To this day, I am still amazed at how many wonderful people know Charlotte.
Charlotte's next MRI is this Thursday, June 16th. Her right leg is about 90% numb and her right arm is about 50% numb, while her left leg is about 40% numb. Her speech continues to decline. I have increased her daily exercise and reading aloud times in hopes of slowing the progression of her clinical symptoms.
I would like to share the following well-written email. The accolades for me are not deserved, but I think the rest of Shelley's writing summarizes perfectly how we all feel when we first hear the word "glioblastoma".
Dear Brent and Charlotte,
My sister Pam was diagnosed with a gbm on April 19th 2011. She is 62 years young and 5 years older than I am. This diagnosis has been the biggest punch in the gut for her family as I am sure is all too familiar with you.
I think I was goggling Avastin, gbm, and diet and your site came up. It really is something what pops up when you least expect it. I have been sitting here at the computer for 3 hours reading your story from the beginning to your latest entry.
You are honest and gentle and human. The love you have Brent for your wife is so apparent and touching. I have welled up many times with tears sitting here reading. A rollercoaster is what you called this journey. Although we have only just begun, the rollercoaster is up and running. We get so excited with the tiniest victory and then sometimes I feel like I just hit a wall. It is so hard to feel balanced....ever.
Pam is halfway through radiation and has been on Temodar since May 6th. She will start Avastin on June 13th. Her husband and I are pretty terrified with the possible side effects. Since her tumor is inoperable, this is the route our Drs have paved out for us. We bought cookbooks for cancer patients and are trying to cook up some yummy cancer fighting food that will help while she is undergoing treatment. We feel utterly helpless.
I wanted you to know how much your posts will help us. There was so much info to absorb, I will have to read it again and again. Brent, I am blown away by the knowledge and patience and dedication to finding the best treatment for Charlotte. I must admit I am intimidated by all the info and websites and terminology you were using. I will have to do some research just to understand some of the words and abbreviations you use. It will be well worth it.
Thank you for all you have done to give hope and understanding to us newcomers to this dreaded disease. God bless you and Charlotte and I will keep you both in my prayers. I have dogs that I love so much and my daughter is an artist. We share some positive things in common, too. :)
Very Sincerely, Shelley (Pam's little sis)



May 27, 2011
Charlotte had her Avastin this morning. Her next Avastin in two weeks (June 10th) will be a busy day for her. We will be attending the Del Mar Fair after her Avastin. Actually we will also be at the artist reception and art preview on the evening of June 9th. Charlotte had three sculptures accepted in the Fine Art show.

May 13, 2011
Charlotte had her Avastin this morning. Her neuropathy and speech continue to be her biggest challenges. She does seem to be a little more fatigued. Her CBC results indicate she probably has a slight viral infection. Her April 21st MRI was read as stable.
I read an interesting study concerning long term survivors (LTS) of glioblastoma. The author pointed out that since the prognosis of GBM patients is so dismal, the treatments at diagnosis seem to include the maximum dosage of radiation and chemotherapy. The study was just showing that these treatments had later consequences. Charlotte's T2 FLAIR on her MRI would confirm treatment damage. Another study said approximately 83% of all long term GBM survivors, defined as living 3 years or longer, suffered from at least one major neurological deficit. Another study was trying to make a mathematical model of glioblastoma patients. The author defined the end of his graph as the "lucky tail". Yet another study revealed how fast LTS seem to perish after a recurrence.
I continue to read as many personal GBM stories as possible. There seems to be no common thread, no magic do's or don'ts. Some long term GBM survivors use complementary/alternative medicine (CAM), just as many do not. Some follow strict diets, others eat anything and everything. Some use off-label drugs, others do not.
My initial impression was that even LTS had a recurrence approximately every two years. Lately I have read of two people that had their first recurrence six years after diagnosis. Even more depressing are those like Mark mentioned in an earlier update. After receiving a "stable" MRI, he was in hospice just ten days later. I am currently following another friend whose last update was Sept 22, 2010. She was ecstatic because her MRI had just come back "clear".
It certainly is not going to change what I do for Charlotte, but perhaps the only common thread among survivors is luck.
I guess that applies to everything in life.

May 3, 2011
Charlotte had her Avastin last Friday, and we saw her neuro-oncologist yesterday morning. Charlotte's April 21st MRI has not been transcribed, so we do not know exactly what the neuroradiologist has written.
I am beginning to see some very slight signs of frustration in Charlotte when she can not find the correct words to express her thoughts. This disease has definitely turned out to be an obvious left side versus right side brain issue. As the speaking frustration is beginning to manifest itself, there is still that joy and tranquility present in her as she creates another beautiful sculpture.

April 15, 2011
Charlotte had her Avastin this morning. Below are photos of her with two of the best nurses at Kaiser. Nori, in the blue gloves, is usually Charlotte's chemo nurse. The other photo is of THE Nancy Grossmann. I know Charlotte would not be with me today if it were not for Nancy's dedication. Thank you for everything Nancy!
The following link was recently posted on one of the brain-tumor research sites. It came with the subject line "Hard to Read". There were a lot of positive remarks posted afterwards, so I am hoping that it may help others during their own brain tumor journey.
Over the past two weeks, Charlotte's speech has continued to decline. Her MRI this Thursday, April 21st, will be coming at a good time.


April 1, 2011
Charlotte had her Avastin this morning (2mg/kg=152mg). Almost immediately after her last update, she started having more speaking problems.She is thinking correctly, but when she verbalizes her thoughts, incorrect nouns replace correct nouns. She will see a woodpecker at the feeder, and say a chicken is at the feeder. She will realize what she said was wrong, and then immediately say the correct word, or think about it for a while to recall the correct word. Sometimes the correct word does not come to her. When she reads aloud, that pathway does not seem to be affected.
We had a very good appointment with her nephrologist on March 24th. Dr Singh came into the room saying she had read Charlotte's last written MRI report, and wanted to learn more about Charlotte's "low dose Avastin" treatment. I understood the terminology; it's just that I had never heard the phrase "low dose Avastin" and glioblastoma used together. I actually had to google them to find out more information.
Charlotte's urine protein had almost doubled last week to 40, but I was able to get it down to 17 in her labs yesterday. Normal is less than 10. My biggest effort has been trying to raise her lymphocyte count. After 26 monthly Temodar treatments, which ended one year ago, her count was around 8 due to the Temodar affecting her bone marrow. Yesterday's labs showed her lymph count to be 18. The low end of normal is 20. Lymphocytes contain T cells, B cells and Natural Killer cells. The NK cells help your body kill cancer cells. Whether NK cells can help "control" glioblastoma cells, I don't know.
I have made a few changes to Charlotte's diet due to their glutamate levels. Chicken broth, asparagus and our home grown tomatoes will be either dropped or reduced. A rush of glutamate is not good for neurological problems, especially in people with disrupted blood-brain barriers.
PubMed has become my home away from home. What a wonderful resource. I am always looking for what might be discovered when you search for glioblastoma and another word, for instance, pAkt. (The combinations are almost limitless.) Charlotte is pAkt positive, which is not good, so I need info on how to control the pAkt pathway. Some abstracts are easy for me to understand, but other abstracts are way above my mental capacity to understand. I also try to look for common threads either running through different abstracts, or make up my own "what if" combinations and feed those into the search box. Maybe I could be more effective at coming up with alternative treatments if I understood more of the terminology.
Before we left for labs and Avastin, I wrote myself the following flow chart "if you decrease fatty acid beta-oxidation, that increases ROS, which decreases ATP, which increases cell death in GBM". I understand all that except for the fatty acid beta-oxidation. I think I had a supplement in mind, but I just can not remember. About 6 months ago I read an abstract about berberine and nexrutine working synergistically to control the pAkt pathway in glioblastomas. I know I read it, but can I find it again? Nope, and that is scary. I can find it for prostate cancer, but not GBMs. Now I automatically bookmark everything.
Charlotte and I did have a few days this week where we only had two walks instead of three. She was finishing a big sculpture in the gallery, and those final days of soldering were long and hard. I put the patina on it yesterday, and it is beautiful.

March 18, 2011
Charlotte had her Avastin this morning. Her GBM recurrence was in March 2010, so we have been blessed that her Avastin monotherapy, along with all of her supplements, have controlled her cancer. I can actually trace her recurrence back to her August 3, 2009 MRI.
Forgetting the last MRI report, these last two weeks have been good weeks for Charlotte. She still struggles with her words, but her labs were all good. I have even been able to reduce some of her BP meds. This has helped stabilize her neuropathy which seemed to be progressing every week.
We have even increased our walks from two to three each day, including a full moonlit walk last night. She does hold onto my arm tighter now, but that just makes me realize even more how lucky we are.
People are like stained-glass windows. They sparkle and shine when the sun is out, but when the darkness sets in, their true beauty is revealed only if there is a light from within.
Elizabeth Kubler Ross

March 7, 2011
Charlotte had her MRI on Thursday, February 24th. I saw my disc copy the following day and thought everything looked stable. Normally I always look at the MRI multiple times over several days to fully comprehend all of the subtle changes. Unfortunately, I only looked at the MRI once this time.
Charlotte had her Avastin on Friday, March 4th, where I was able to obtain the written MRI report. The neuroradiologist said "their appears to be subtle T1 pre and post contrast hyperintensity and cannot exclude a subtle degree of enhancement". She does remark in her summary that there are "no significant changes to the last brain MRI". Charlotte and I spent all day Saturday and Sunday reviewing her MRI. We knew we had an appointment today with the neuro-oncologist, and we wanted to be prepared. We always try to go over all of our options ahead of time, and rank them accordingly. We then listen to the neuro-oncologist, and then finalize our decision.
In this case, we've decided on a "watch and wait" approach. Her next MRI should be on April 21st.

February 18, 2011
Charlotte had her Avastin this morning. Her labs yesterday and her BP this morning were all pretty good. But her neuropathy in her legs continues to increase making her walking more difficult. We still go for a walk in the morning to visit all of our lovers before going to the gallery, and repeat everything when we return in the afternoon. The walk is slightly uphill until we get to everyone, so it is good for both her legs and her cardiovascular system.
Charlotte always called our gallery "a place of hope and joy". We have been very fortunate that it attracts people desiring those same inner feelings. I personally would like to thank everyone for visiting the gallery, and for their heartfelt emails and support.
Charlotte usually walks to the front of the gallery to greet visitors, while I remain behind working. Last week Charlotte talked with a gentleman for quite a while before I walked past them and he made the comment "I love your wife..." As time went on, I passed them again and this time he said "I really love your wife..." As he later explained, he read and studied the philosophies of the world, especially Buddhism. Even though they had just met, he felt Charlotte had tremendous "inner peace and strength, along with other wonderful traits".
We are blessed by having such visitors.
Charlotte's next MRI is this Thursday, February 24th, at 8:45pm.

February 4, 2011
Charlotte had her Avastin this morning. The neuropathy in her legs continues to increase, as well as her difficulty in finding the correct word when she speaks. However, her labs yesterday finally showed a slight improvement in her kidney function. I am trying to decrease one of her BP meds, which should also help her kidneys. I failed in my last attempt because her BP continued to rise.
Our neighbor Dora Myrick chose her words carefully this week when she told Charlotte that although she always looks good, she looked liked her "old self today". I heard several similar comments this week. I agree than on certain days she does have that healthy glow.
Charlotte's love for life and her determination to be a long term survivor is truly inspiring. She never complains about anything, including her exercises, walks, supplements, etc. I have added many new supplements, and have significantly increased the dosage of some of her existing supplements during the past month.
However, she does complain about the broccoli seeds in the bottom of her drinks!
Charlotte also knows how fast her condition can change, but she accepts it and somehow uses it in a beneficial way. She often jests with other patients that "she is the only one left above the sod". It is always said in a positive manner, and usually to someone that she is trying to inspire. It's hard to explain, but the beauty in her has never waned during these past three years. This week her beauty seemed to peek through just a little more.

January 21, 2010
Charlotte had her Avastin today. There has been a trend in her labs over the past month that has me concerned.
Four weeks ago there was a decline in her kidney function as indicated by her serum creatinine results. The initial decline remained constant for the following two weeks, but then it declined even further yesterday. Her BUN ( blood urea nitrogen) test two weeks ago was 25, normal being less than 19. A high protein diet can be one cause of an elevated result, so I stopped her whey protein for a week and the result yesterday was 17. Both of the above tests measure kidney function, but each test has different conditions that affect the results.
All of her past serum creatinine results, and her GFR (glomerular filtration rate), were definitely caused by her Avastin. Besides the Avastin, I'm hoping there might be a "minor", less insidious contributing factor this time. Her blood pressure (BP) has been nice and low lately. But sometimes I think it might be a tad too low, even though she never has hypotension (BP 90/60). I have tried cutting back on just one of her BP pills, but her BP immediately rises again, which then translates into a higher UPC ratio in her next labs.
One reading that I had never seen before was her pulse rate of 46 in the chemo room today. I'll have to check with her nephrologist, but I believe her pulse rate should be above 55. Low BP can be just as harmful to the kidneys as high BP. I don't know if her pulse rate can be too low for correct kidney function.
We both had our teeth cleaned on Thursday by our friend Grace Hansen. A comparable picture to the one below was in the May 5, 2009 update. I think both Charlotte and Grace look as beautiful as ever!

January 10, 2011
Charlotte had her Avastin on Friday, Jan 7th. We met with her neuro-oncologist this morning. I was mainly looking forward to receiving the written MRI report. I had reviewed my disc copy of her Dec 30th MRI, but had difficulty reading the T2 and T2 FLAIR images, which are the important images when taking Avastin as a monotherapy. Two years ago Kaiser included a "slideshow" program in their MRI disc that you could speed-up or slow down the images. They dropped that feature so images are only viewed "statically" now. Every time I looked at the T2 and T2 FLAIR images, my opinion slightly changed, and I wished I had that "slideshow" feature. As it turned out, the neuroradiologist read everything as stable.
I did go back this week and looked at Charlotte's MRI on 3-14-2010 which showed her recurrence. I had forgotten how big and multifocal the tumors appeared. Really scary! She started Avastin (2mg/kg) immediately as a monotherapy (not counting her many, many supplements) and her 4-11-2010 MRI thankfully showed some improvement. She has had 6 MRIs since April, and everything has been stable.
I have been critical of Avastin in the past, but it is currently a miracle drug for Charlotte. I just hope it continues to be effective. However, I read a study presented in the January 2011 issue of BrainLife.org that starts with the sentence " There is no effective treatment for recurrent glioblastoma (GBM) after bevacizumab (Avastin) failure."
A very sobering sentence to read and comprehend....
Charlotte's immediate concerns are pill fatigue, her walking ability and her correct "word-finding ability". We continue to go for 1-2 walks everyday (weather permitting) to help her with her walking. I've noticed she does have a firmer grip on my arm these days. Her language still seems to suffer from either nonenhancing tumor and/or postoperative effects. Her other cognitive abilities have never been affected.
She still works everyday at the gallery when we are not at medical appointments. Her artwork still remains unique and beautiful. Sort of like her!

December 23, 2010
Charlotte had her labs yesterday and her Avastin today. Both are a day early this week because the chemo room will be closed Dec 24th.
Charlotte spent about 8 hours in the ER on Monday due to severe vertigo that was causing nausea and vomiting.
We finally left with a scopolamine skin patch behind her right ear, and were told to come back in three days if the symptoms did not improve. The patch also lasts for three days, so I presume we would have waited another 8 hours for another patch if the symptoms were still present. The symptoms are getting better, but are not gone. I have her on Bonine, which is an OTC med for motion sickness. Her official diagnoses is BPPV (benign paroxysmal positional vertigo). Research told me it could last for a couple of weeks.
We also met Charlotte's new nephrologist on Wed. I had a special relationship with her old nephrologist when it came to administering BP meds while she is on Avastin. Our new nephrologist seems to be even better at trusting my judgment. Most doctors never understood how fast Avastin can create hypertension. A few months ago I read a clinical study that said Avastin causes hypertension after taking it for 6-8 months, and then it lasts for approximately 12 months, even if you stop the Avastin or dramatically increase your BP meds. Those dates coincided exactly with my records when Charlotte was on Avastin during the UCLA/Kaiser study trial in 2008 and 2009. The high blood pressure leads to a high UPC ratio, which finally made Charlotte drop out of the study trial. She started Avastin again in April 2010 after her recurrence, so I knew it was only a matter of time before her BP would be out of control again. That came true 6 weeks ago. Finally, after doing what I thought was necessary for the past 6 weeks, her UPC ratio took a big drop in her most recent labs. Her BP is also currently under control, and that is always my leading indicator of things to come.
I was going to add more of my opinions from the release of Charlotte's UCLA/Kaiser study trial in the Journal of Clinical Oncology. Please see my last update for my initial thoughts. I will add more next time, but I have also decided not to mention some statistics that did not affect Charlotte negatively (e.g. MGMT promoter methylation status), but did affect many others. I still believe certain people should not have been allowed to participate, or at least made sure they had the same information that I requested from UCLA 3 years ago.
The newest fact that I learned was that their were two arms in this study. One arm was given surgery, radiation, Temodar and Avastin. The second arm was given surgery, radiation and Temodar (but not Avastin). Those that were given upfront Avastin had a better outcome for the first 16 months, but then they had a poorer outcome than those not receiving upfront Avastin. Charlotte was in the arm taking upfront Avastin. She took it for 15 months, so I guess that is good news.
Charlotte's next MRI is this Thursday, Dec 30th at 8pm.
December 10, 2010
Charlotte had her Avastin this morning.
Her labs on Thursday showed the Avastin is still causing proteinuria. It has dramatically increased over the last 4 weeks. Her neuropathy in her right leg is almost 100% now, and her ability to find the correct word in her speech has continued to decline. This week was also the first time that Charlotte began to complain about "pill fatigue". She takes 40+ pills 3X a day with her meals, and then 30+ pills 2X a day on an empty stomach.
"Traditional cancer treatments have only focused on the cancer cells, leaving the cancer stem cells behind. Chemotherapy will kill cancer cells, but cancer stem cells may somehow "hide" during chemo or radiation, then later they morph into actively growing cancer cells. If even one cancer stem cell survives, you're going to have an entire tumor reconstituted, and in a more aggressive form. So in addition to killing cancer cells, cancer treatments must target cancer stem cells to eradicate the disease before they get a chance to initiate new patterns of growth and cause even more problems. If you kill the cancer stem cells, then you eradicate (cure) the cancer."
When I read about cancer stem cells and the pathways that they may take, such as AKT, NOTCH, etc, it is hard not to do hours of research about clinical trials on PubMed and try to find some answers on how to control these pathways. If I'm lucky, that leads to more pills. Technically, Charlotte is not taking any chemo that kills cancer cells. Avastin just controls the blood supply to the tumor. By using off-label drugs and supplements, our goal is to keep her cancer cells under control. That means keeping her brain cancer from enhancing, spreading, or becoming diffuse. She agrees that a few extra pills are worth taking if they keep her from having to go back on chemo with all of its side effects.
I'll give more details in my next update, but the results of the phase ll study of Temodar/Avastin at UCLA/Kaiser that Charlotte participated in were finally published in the Journal of Clinical Oncology on Dec 10th. I've read the results, but I always rely on brain tumor research sites for experts to express their opinions. I'll only say, that in my opinion, the overall survival results in this trial were not impressive.

November 28, 2010
Charlotte had her Avastin on Friday, Nov 26th. She received an extra long "I.V. flush" after her Avastin in hopes of stopping her headaches, nausea and vomiting. We were thankful it worked because Charlotte read poetry the following night at the Julian Christmas Tree Lighting Ceremony. This update could continue with Charlotte's bad lab results, the effects of the Avastin on her body, etc.
Instead, last night's wonderful poetry reading was a time for us to celebrate and to give thanks for these past three years. The poetry reading marked Charlotte's third anniversary of being diagnosed with brain cancer.
Thank you everyone.

November 16, 2010
I am a little late writing this update, but after studying Charlotte's Nov 4th brain MRI for about 8 hours a day for over a week, I still could not decide on what exactly was being displayed. I immediately knew it was not as "clean" as her previous MRIs. I wanted to read the written MRI, plus see a another doctor before forming my opinion.
Before going any further, I would like to say that there are at least two things that I have always avoided in these updates. One is that about 95% of what I do medically for Charlotte is never mentioned because of ethical reasons. I also do not mention doctor's personalities. Both of these would be very unprofessional of me.
First, I found two areas of concern that the written MRI did not even mention. The other doctor agreed with my concerns. Second, Charlotte's neuropathy in her right leg has dramatically increased from 80% two months ago to 95%. Walking is extremely hard and dangerous for her. Third, her UPC ratio doubled in the last week. It is now the highest it has been since early June. Fourth, and this relates to her UPC ratio, her BP has been out of control since her last Avastin treatment on Friday. Also since Friday, she has had nausea and vomiting.

October 29, 2010
Charlotte had her 15th Avastin treatment today since her tumor recurrence. Her next MRI will be this Thursday, Nov. 4th, at 8:45pm. It's been 60 days since her last MRI, so I don't know what I'll see on her MRI on Friday. Her recurrence in March was on a 30 day MRI, and it showed a golf ball size tumor with many other diffuse lesions. Surprisingly she showed no clinical symptoms then, and is basically showing "none" now . She still has neuropathy, speech and memory problems, but as time goes on and her MRIs remain stable, I'm beginning to blame these deficits as much on her treatments as on her residual tumor. Then again, the Avastin could be cloaking new tumor, and all heck could break loose at any time.
I picked the picture below to remind me that I should keep as much sadness and stress from Charlotte. She has to keep that positive attitude that she has been blessed with for the past three years. There has been a lot of things going on in our lives right now that is causing her stress. I feel she might even have some depression. Even though she shares her thoughts with me, I know she wishes she could convey them more clearly to others. Losing Alpha to cancer was only the beginning. But we have two strong antidotes to our situations.
First, Charlotte, like her mom, is a fighter.
Second, we are, and always will be, a team.
We will continue to make life's journey together.
October 15, 2010
Charlotte had her Avastin this morning. Her UPC ratio, which I thought I had under control, seems to increasing again. Her neuropathy has also increased, especially in her right lower leg. She is now 90% numb which makes walking very difficult and dangerous for her.
On Monday, Oct 4th, Charlotte and I held in our arms our youngest and most precious dog "Alpha" as she was put to sleep. She was 15 pounds of pure love and joy, and just shy of being 6 years old. She had a bleeding cancer mass in her abdomen, and it had also metastasized to her liver. We buried her on a cold and rainy day in our pet cemetery, along with her favorite toys. Mommy says she knows we will all be together again someday.
October 1, 2010
Charlotte had her Avastin this morning. She still has:
1) numbness (85% in her right foot/lower leg and 10% in her left foot, along with 25% in her right hand)
2) speech and short term memory problems.
Her speaking problem has slightly increased since her last update, but I would not call it a dramatic change.
I increased her hydralazine (BP med) from 50mg to 60mg three weeks ago, and the upward trend in her UPC ratio stopped this week. Hopefully this week's ratio change was not a one time abnormality and will not continue to increase in the future. Her Avastin, hydralazine and statin meds have all been associated with neuropathy, so it is definitely a "catch-22" situation.
Other than the above problems, she seems to be doing fine.
Charlotte's next MRI is scheduled for November 4th at 8:30pm. We will see her neuro-oncologist eleven days later. I requested that schedule for her last MRI, which made the written MRI report available to me before the oncology appointment. That just gives me more information and to be better prepared for our consultation.
I need to add one addition to my "behavioral changes" when it comes to Charlotte's MRIs. In my last update I mentioned just two or three instances that affected me. Those events seemed to make my stress level go up and my behavior change. They were the actual MRI, my first look at the MRI and obviously hoping to see no enhancement, and then waiting for the written MRI report, which can take from seven to ten days. Actually each of those individual events is not that intolerable. What I failed to mention was our visit with the neuro-oncologist.
So far we have been extremely lucky. Temodar and Avastin are the best drugs for Charlotte. She failed Temodar in March, so trying Avastin again was our obvious next choice. We have been very lucky with the Avastin, especially at 2mg/kg. But I know she will eventually fail Avastin too. I do not have an obvious treatment plan once this happens, and that is what scares me. There are many older chemo drugs available, and they will undoubtedly be suggested, but the statistics just don't back up their effectiveness. There are some off-label drugs that have proven effective for some glioblastoma patients, but you need to have an understanding neuro-oncologist to prescribe them. That usually never happens.
Charlotte's body has endured almost three years of therapy, and I know she could not handle any of the more toxic chemo drugs. She always says "we'll do whatever needs to be done". But I know that our options will be very limited, and that is obviously very stressful. But then I remember Tom's words... "there is always someone worse off than me..." I KNOW how blessed I am to still have my soulmate
 . .
September 17, 2010
Charlotte had her Avastin (2mg/kg) this morning. Our "angel" Nancy Grossmann gave me Charlotte's written MRI report, along with some CBC results that I can not access at kp.org. Basically the MRI report confirmed what I had seen on my copy. Some things looked a tad better, and a few things looked maybe a tad worse. As I mentioned in my update prior to her MRI, there were a few clinical symptoms that concerned me. Foremost was Charlotte's neuropathy (now in both legs) along with an upward trend in Charlotte's UPC ratio. The Avastin is responsible for the UPC ratio, and is the main contributor to her neuropathy as well. Charlotte's BP med hydralazine can also cause neuropathy. Her speech and memory problems could be due to tumor recurrence that we just don't see because of the Avastin cloaking the tumor. Even though I have many misgivings about Avastin (March 5, 2009 update), I am truly thankful for it now.
Now a little bit about this whole MRI experience and glioblastoma. I always think of Tom and Mary Oppenheimer, and Mary's remark that the 7-10 days of waiting for the written results after Tom's MRI were becoming "unbearable". Actually, for me it has become "pure hell". And I'm even able to read the MRI disk the day after Charlotte's MRI to help form an opinion. About one week before an upcoming MRI, I really start to change. It didn't help this time that I had just read about another 4 year survivor friend dying suddenly (not Mark). My attitude change has happened before with previous MRIs, but it is getting worse with each new MRI. I KNEW I was changing and had to sit down with Charlotte to apologize for my behavior. The conversation ended with her trying to apologizing to me! But it is amazing how stressful those 2-3 weeks have become around a scheduled MRI. And it is stressful for both of us. I'll never forget how happy Charlotte looked when I finally came into her room and told her "everything looks stable". I know she worries about me too, both short-term and long-term, and is under the same amount of stress.
One note about my last update and the e-mail from Tom Oppenheimer's daughter Susan.
Susan, I think about your line "my dad would always say, there is always someone worse off than me...".
I have found much comfort in that line, along with your entire e-mail during these past few weeks.
The lines from Invictus have also given me strength.
I can tell you are dad's daughter.
Thank you.

September 3, 2010
Charlotte had her Avastin this morning. There are a few things that worry me:
1) Her labs yesterday showed another decrease in her urine creatinine, which in turn raises her UPC ratio. The UPC ratio has been steadily rising and the upward trend concerns me.
2) For some reason Charlotte's gait has now started to become more of a shuffle.
3) Finally, her right lower leg has been about 70% numb for quite a while; hence her walking problems. Now her lower left leg is about 30% numb.
Her next MRI is Thursday night, so I'll wait for that information before I make any decisions.
I received quite a few wonderful e-mails this week regarding my last update. One was from Tom Oppenheimer's daughter Susan. She gave me permission to share her thoughts.
Please see the Nov 12th 2009 and Nov 19th 2009 updates on Tom.
Hello,
I am the daughter of Tom Oppenheimer and from time to time read your posting on Charlotte and I just want to say that as I sit on the sidelines wishing for Charlotte's recovery. I think it is important for you to know that you both are an inspiration. Thank you!
It has been almost 10 months since I lost my dad, and I would trade spots with you in a moment, because although the highs aren't as high and the lows are lower, you still have the courage to fight and the hope and determination to succeed.
My Dad would always say, there is always someone worse off than me, usually it was when he was on Chemo and he was at his worse. It has almost been three years, it is hard to feel fresh and on top of it and I am sure you are both tired, but stay the course. I have always believed in what you two have decided to do together with and without the Doctors blessing.
Just a final thought taken from the movie Invictus, to help keep that fire burning and to carry you to victory.
Out of the night that covers me,
Black as the Pit from pole to pole,
I thank whatever gods may be
For my unconquerable soul.
In the fell clutch of circumstance
I have not winced nor cried aloud.
Under the bludgeoning of chance
My head is bloody, but unbowed.
Beyond this place of wrath and tears
Looms but the Horror of the shade,
And yet the menace of the years
Finds, and shall find, me unafraid.
It matters not how strait the gate,
How charged with punishments the scroll.
I am the master of my fate:
I am the captain of my soul.
I thought I had learned all I could at the age of 45 from my Dad, boy was I mistaken, he had one more thing to teach me, and I will forever be grateful.
The bravery and the courage both Charlotte and my Dad have displayed is truly something we all can learn from. Keep up the fight!
All My Best,
Susan

August 20, 2010
Today Charlotte had her tenth cycle of Avastin since her recurrence back in April. Her next brain MRI will be important because the PFS (progression free survival) for GBM patients when taking Avastin as a monotherapy upon recurrence of the tumor is approximately six months. Her next MRI is scheduled for Thursday evening, Sept. 9th. That will be just about six months for the Avastin. April's MRI was absolutely horrible, but you can go back to the Dec MRI and see the first signs of tumor growth.
But now to the positive. Charlotte is still having her usual speech, memory and walking problems, but she is trying her darndest to keep getting stronger. She has actually sneaked out with the dogs and gone for a few very short walks. She always holds onto my arm when we're together, but she now feels comfortable doing some of these walks on her own.
These past 32 months have been a roller coaster in everyway imaginable. I told someone a while back that it was like a roller coaster, but I just felt our highs were not as high as they were in the past, while our lows were seemly getting lower.
But just within the last week I think Charlotte looks as healthy as anytime in the past. (July 9, 2009 is still her heathiest picture.) I don't want to put a curse on things because I also felt she was doing well in April just before her terrible MRI.
I have made some major changes in her supplements since April, so perhaps that could be one reason. I have also been giving her, for instance, whey protein, for all of its immune benefits. But I still can not get her lymphocyte level back to normal, which is my number one priority right now. The two big suppliers of nourishment for brain cancer cells are glucose and glutamate. Whey protein is very high in glutathione, thus glutamate. (Yes, I could be fueling her tumor, but see my remarks below about "thinking outside of the box".) One of my many conundrums is when to give her the whey protein and colostrum. They are to be given on an empty stomach. But so is her IP-6 and inositol, and both of those combine readily with protein to make the IP-6 ineffective. Now she gets her colostrum with her BP meds one hour before breakfast. Her IP-6 and inositol are given with her other empty stomach pills. The whey protein is given with meals, even though it makes it less effective.
I decided 28 months ago to do everything possible for Charlotte, because the statistics for glioblastoma multiforme are dismal. Just 2-3 people knew exactly what I was doing, and I certainly didn't put anything in my updates until last time when I mentioned that she took 25-30 pills 5 times a day. I still have no idea if anything that I have done has been effective, so that is why I still keep my ideas to myself. I remember reading on one website where the husband "had spent thousands of hours researching and thousands of dollars on supplements trying to save his wife". He was quick to point out that there were no clinical trials that supported any of his efforts, but that didn't matter to him. It was just something he had to do. I feel exactly the same way.
I do try to "think outside of the box", but when I talk with Charlotte about possibly being wrong, she always reminds me to "never second guess myself when things eventually turn against us. We gave it our best shot."

August 6, 2010
Charlotte had her Avastin this morning. A few days after her last Avastin, she came down with the "flu". She did not eat any solid food for four days, but did have an Ensure at mealtimes. I became worried that her blood counts might be too low for the Avastin today, but everything seems fine.
I was asked last weekend about writing a separate update on Charlotte's MRI results. I do mention them in her regular updates, but since a MRI is basically just a snapshot in time of her brain, I feel sometimes that a "stable" MRI can make you feel too optimistic. Mark's updates on his website which I mentioned in my last two updates are a perfect example. One reason that I was so sad after his death was that I reread some of his earlier updates. Some included his MRI images, and they usually always showed great improvement from his latest GBM therapy. I have read similar results on other sites too, and then things take a dramatic turn for the worse. Charlotte and I have learned that this is how this disease works, but that doesn't keep us from trying everything we can to stay one step ahead of this cancer. I know a brain researcher that changes his wife's chemo every 12 months just to keep her GBM cancer cells from adjusting to her treatments. His wife has had "clean" MRI scans for almost three years now. I don't know if I would have the nerve to change treatments for Charlotte if her MRIs were showing no tumor. (I guess that is what a "clean" MRI means, although having a GBM and then no tumor sounds like an oxymoron to me).
I did receive Charlotte's written report on her last MRI today. It is "stable", but she still shows areas of tumor mainly along the margins of her surgical cavity. There are also other areas "of concern", but all areas show no major changes since her last MRI.
I had to laugh yesterday with Charlotte after Avastin. We were having a flat tire on our car repaired in Ramona when she said "I don't see how you do all this". I had just explained to the tire person that I would like to keep my wife, who had just finished her chemo, along with our five dogs, in the car while they worked on the tire. Plus I wanted to keep the car engine running in order to keep everyone cool, along with our groceries. The tire company was family run so I knew they would understand.
Anyway, there were other things that I had forgotten that I thought were pretty major, but Charlotte, in her usual loving way, tried to put everything in perspective for me and told me just how lucky we are in life. She repeated how she didn't know how I managed to do everything. I told her she was my inspiration. Never once have I heard her complain about anything in these last 32 months. She's the one that takes 25-30 pills 5 times a day with special drinks, eats meals that follow a very strict diet, has nausea and vomiting following certain chemo treatments, etc, etc, etc.
I won't even mention the kiln loads of artwork that didn't turn out correctly. She says "a mistake is always a new opportunity for our sculptures".
I am truly the luckiest guy in this world.

July 23, 2010
Charlotte had her Avastin this morning. I think her clinical symptoms are about the same as they were two weeks ago. Her remembering the correct words might have slightly declined when she speaks, so her brain MRI this Sunday night is coming at a good time. We have been doing more specific exercises to help strengthen her arms and legs, and those have already made a noticeable difference. Her labs continue to be good. In fact her urine protein came back at 30 yesterday, which is the lowest it has been in over two years.
It has been as high as 225 during those two years. The lower dosage (2.0mg/kg) of Avastin certainly helps, but I just hope her next MRI shows that the Avastin has also been controlling the tumor.
The weather was very hot last week, so we decided to stay in our cabin and to work with clay. The clay pieces will be combined with glass in some new sculptures.
I had lots of comments about Mark in my last update. Some people had missed the fact that it was only 12 days between his stable MRI and his last MRI that showed 4 new tumors combined with new lesions. I actually visited his site again last night just to see how he was doing, and to read more of the vast information that he had accumulated. It was a sad night for me.
Please visit Mark's wife Rachael and her lastest post.

July 9, 2010
Charlotte had her Avastin (2.0mg/kg) this morning.
As I stated two weeks ago, her biggest two problems continue to be trying to remember the correct word when she speaks, and her walking ability due to the numbness in her right leg. Both of these have remained about the same over the past two weeks. Her labs have been good since she restarted Avastin in April. Her urine protein levels have remained about the same which is definitely good news.
What wasn't good news was reading about Mark.
I do visit other brain cancer patient websites, and when I visited his site about two weeks ago, I was devastated. Mark is a three year GBM survivor with a beautiful family. I was first attracted to his site because somehow he was able to post his own MRIs, etc. Anyway, you can click on his five "recent posts" listed on the left side to understand how fast this terrible disease can ruin your life and those of your loved ones.
God bless you Mark, Rachael and family.

June 25, 2010
Charlotte had her Avastin (2.0mg/kg) today. Overall, I think she is doing fine. Two things do worry me though.
First, her speech, short term memory and walking ability still seem to be slightly declining. Second, her last MRI (6/17/10) came back "abnormal". I don't have the written report, so I won't speculate on what is in it. Dr Spier did say one view, the DWI (diffusion weighted imaging) is what concerned the neuroradiologist. He saw some previous spots the were larger and more intense. DWI usually shows a brain ischemic stroke, but I have since learned that it could also show tumor when interpreted with the ADC (apparent diffusion coefficient) map.
Her next MRI will be on Sunday, July 25th.
Another good series of brain cancer videos are found at www.virtualtrials.com. The videos educate you on various brain cancers, conventional therapies, nutrition and supplements, other alternative treatments, etc. The nutrition and supplement videos are appropriate for those with other cancers.

June 11, 2010
It was a full day for Charlotte today. She had her Avastin at 8am, which usually takes about two hours. We then met Donna and we all proceeded to have a wonderful day at the Del Mar Fair. This year we enjoyed the "dog show" held in one of the big arenas. We watched mainly border collies doing all kinds of agility contests. It started at 3pm, which is our normal time for leaving, but we watched all the agility contests for the next four hours!
Charlotte will have her brain MRI this Thursday.
Here is an interesting video link that was just recently sent to me.
http://www.ted.com/talks/william_li.html I learned about these concepts over two years ago and they are part of Charlotte's treatment plan.

May 28, 2010
Charlotte had her 4th Avastin infusion this morning. Last October she received 4 Avastin treatments before her blood pressure and UPC ratio dramatically increased and kept her from receiving any further Avastin treatments. It took about 4-5 months for her UPC ratio to fall below 2.5. Her BP, UPC ratio and Avastin dosage are all comparatively lower than they were back in October, so I'm keeping my fingers crossed.
Last Tuesday and Wednesday Charlotte and I worked on a clay torso in our cabin. We decided not to go to the gallery in order to keep a watchful eye on Sadie, one of our 5 dogs. We believe she received a "glancing" rattlesnake bite early Monday morning. We didn't even realize she had been bitten until we came home from the gallery at 5pm. She was very swollen on her nose and lower throat, but was very energetic and able to eat and drink normally. We were very lucky this time. Alpha, our smallest dog, was bitten about 3 years ago and needed 2-3 vials of rattlesnake antivenom.
After her Avastin 2 weeks ago, Charlotte seemed to have a lot more difficulty with her speech. She was fully aware of her speech problems, and would say "what is the matter with me?" She still uses a wheelchair for long distances, and a cane for shorter trips. Numbness in her right leg makes walking difficult, but she does surprise me at times. She just walked around Costco with me after her Avastin. There is also some slight numbness in her right hand.
Charlotte has an appointment with the nephrologist next Friday, and another brain MRI on Thursday, June 17th, at 7:45pm.

May 14, 2010
Charlotte had her third Avastin infusion this morning. She will continue receiving Avastin as a monotherapy every two weeks at 2mg/kg (normal is 10mg/kg) as long as her UPC ratio remains below 2.5. Charlotte's MRI last Sunday showed that the Avastin was controlling her new tumors. I normally have a bad opinion of Avastin, but right now it is our only choice.
Charlotte's next important appointments will be with her nephrologist on June 4th, another brain MRI the week of June 13th, and then Dr Spier (neuro-oncologist) on June 21st.

April 30, 2010
Charlotte had her second Avastin treatment this morning.
We made a decision two weeks ago after her first Avastin treatment not to start the etoposide. Charlotte's kidney health is most important if she is to continue with Avastin. The etoposide does affect renal function, plus I discovered a clinical trial from Duke University that found there was no difference in a recurrent GBM between using Avastin as a monotherapy and using Avastin combined with etoposide. We only have a 30-40% chance that Avastin will even control the tumor for a few months. It's probably even lower than that because Avastin is most effective for solid tumors, not diffuse tumors.
I told Charlotte that the worst news we could hear is that the Avastin is controlling tumor growth, but she could not continue to receive it because of her kidneys. She took Avastin last November and was only able to receive four treatments before it was discontinued.
It's hard to accept, but Temodar and Avastin are currently the only effective drugs. Everything else is an older drug that neuro oncologists will prescribe, but will usually not be effective but will only have harsh side effects.I've read too many stories of patients just getting sicker because of these chemo's. Charlotte might have a new tumors, but because of their location, she currently has no clinical symptoms and she is feeling fine. I want to try and keep it that way for as long as I can. Her tumor locations also rule out any further surgery or radiation. Her next MRI is on Mother's Day, May 9th. All we are hoping for is a MRI that shows "controlled tumors".
Last week Charlotte and I had a wonderful time working in the gallery. We both worked on separate but similar freestanding sculptures. She did her interpretation with the glass pieces, and I did mine. About every hour or so, we would discuss the shapes and colors in our sculptures, and our reasoning behind everything.
We talked "sculpture", and that was wonderful!

April 15, 2010
Charlotte had her MRI late Sunday (April 11th).
On Monday, I saw that her tumors had at least doubled in size during the past 30 days. I again wanted to carefully review everything with her and to talk openly about our options before our meeting with Dr Spier on Wednesday.
Charlotte and I decided to try Avastin again at 2mg/kg in hopes of preserving her kidneys. We also have added oral Etoposide and dropped the Temodar. Both the Avastin (every two weeks) and Etoposide (21 days on, 7 days off) begin tomorrow.
Her next MRI in 30 days will hopefully show some tumor stabilization. If not, we will switch chemotherapies again if her tumor progression allows us to make another change.

March 17, 2010
Charlotte will restart her Temodar tonight. We received the dreaded phone call late yesterday from a secretary informing us that Dr Spier wanted to see us today. Our normal appointment would have been next Monday. I knew immediately that the radiologist must have read Charlotte's MRI as "abnormal".
Charlotte was working next to me when I received the phone call. You could immediately see all the hope and joy drain from her face, and fear starting to creep into her eyes. We immediately closed the gallery and went back to the cabin. I wanted her to be with me as we reviewed her latest MRI together.
She had her MRI late on Sunday, March 14th, and I picked up my copy on Monday. The first view that I usually look at is the AX T1 POST, which scared me too. It was definitely "brighter", but that doesn't necessarily mean tumor growth. Still, not a good beginning! I took my time reading all of the other views, AX T1, AX T2, AX T2 FLAIR, COR T1 F/S POST, SAG T1 F/S POST, etc. Plus I kept coming back to view the images during the day because I don't comprehend everything at one sitting. On Tuesday I had told Charlotte that except for one view, I thought she was stable. That was before the phone call.
After closing the gallery, Charlotte and I reviewed her MRI for about an hour. I wanted her to know exactly what the MRI showed, and why the radiologist read it as "abnormal". I had to go all the way back to her Sept 2009 MRI to really compare "apples to apples". All of her previous 8 MRIs just didn't line up correctly for comparison, plus she had been on Avastin. We talked about what might be discussed with Dr Spier tomorrow, and what would be the best course of action. Charlotte decided to restart Temodar. She also felt more comfortable her MRI results.
Dr Spier agreed with restarting the Temodar. She even agreed with my MRI comparison of March 2010 versus September 2009 (about looking the same), and suggested that Charlotte might even try staying off chemo for one more month, or longer, until the MRI showed progression. That was obviously not acceptable to us.There is no "correct path" during this journey. You just have to do what you think is best, and remain flexible. Circumstances can, and do, change very fast.

February 25, 2010
Charlotte will not be having her Temodar tonight. Temodar is usually given only for a maximum of 24 cycles due to its toxicity. This would have been Charlotte's 26th cycle, and Dr Spier on Monday gave us two options. One was to continue the Temodar, but Charlotte would go back to having a MRI every 60 days. The other option would be to stop Temodar, but to continue the 30 day MRIs for at least another 3 months in hopes of catching any tumor enhancement.
Charlotte and I have talked about going off Temodar just to give her body a chance to recover. She did not want to do it last month, but she felt this month she would give it a try.
The cons of the above decision are:
Charlotte and I both know she still has cancer cells in her brain and that the tumor will eventually return. Dropping all chemo may make the tumor reappear with a vengeance. A recurrent GBM is usually always fatal within months.
Enough said on that ...
The pros would include:
The tumor remains stable, and Charlotte's body would grow stronger. And when the tumor does reappear, "hopefully" it would show itself as slow enhancement on her MRI, which would "hopefully" allow us to get the tumor under control again. And "hopefully" it would not be as medial as her 7mm "hot spot" on her PET scan as compared to her old tumor bed.
For months now, I have actually been more concerned with trying to get Charlotte's kidneys healthy.
I have visited too many websites where the patient succumbs to the effects of the chemo treatments, but are basically cancer free.
I have also been trying to prioritize our time better. Because of her clinical symptoms, I believe the best medicine for her is to work on her art as much as possible, to "walk" as much as possible, and to have the occasional short talk with customers to help her speech. Her gallery is the best place for her to be right now. Her art is not only exquisite, but I think it is good therapy for all of us!
I do not have the written report for Charlotte's latest MRI which was last Friday (Feb 22), but it looks stable again. The problem that everyone is having is that MRIs are a wonderful diagnostic tool from the head down, but it is a different story when the head is involved. It is really hard to say exactly what Charlotte's MRIs are showing us. It could be tumor, scar tissue, radiation necrosis, etc. Even with Charlotte's PET scan (Sept 14, 2009) that showed a 7mm "hot spot", one doctor told me "if we can believe this scan..."
Charlotte's clinical symptoms are about the same as they were a month ago. She still uses a wheelchair at times, but she now uses her cane and not a walker for short distances. Her speech is also about the same as a month ago.
Thank you to our neighbors Al and Dora for being our "chauffeurs" for two weeks while our car was in the shop.
And a special thank you to Dr Iris Lowe for working so diligently on Charlotte every week. Even though we can not spend as much time together as we would like, thank you Donna for showing up at Dr Lowe's every week just to be with Charlotte.

January 28, 2010
Charlotte starts her Temodar tonight. Her UPC (urine protein creatinine) ratio is still too high to restart her Avastin. Her labs yesterday showed her UPC ratio, instead of steadily decreasing and getting better since her last Avastin, had increased from 2.9 to 3.6 just in the past week. I believe her kidneys (e.g. Avastin) are a large contributor to the problems that she has been having during the past 30 days. Last month she started using her mother's cane in order to walk. When we saw Dr Spier this past Monday, Charlotte asked for a wheelchair. She also used one for her labs yesterday.
She had a brain MRI and a cervical spine MRI on the 22nd. I don't have the written reports yet, but this is what Dr Spier said on Monday. First, her cervical spine MRI did show some problem areas, but probably not enough to account for Charlotte's numbness in her right arm and leg. The brain MRI was stable in the T1, T2 and FLAIR sequences, but the technician used "fat saturation" in all of the contrast sequences that made them useless for comparison.
Charlotte now wants to see her chiropractor, Dr Iris Lowe, once a week. Last Thursday Charlotte walked into Dr Lowe's office using her cane, and walked out without needing it. She did walk a long way with her cane last Friday for her MRI before asking for the wheelchair on Monday. Dr Lowe wanted a "lumbosacral with femurs" MRI. That will be done along with a brain MRI and a brain MRA in 30 days. The MRA (magnetic resonance angiography) is for diagnosing a possible bulging artery/vein.
For the past 30 days I have seen a decrease in both Charlotte's walking and speaking ability. Dr Spier says it can be the result of tumor progression and/or the effects of Charlotte's radiation and chemo treatments. The walking and speaking problems could be the early clinical signs that appear before the MRI reveals tumor progression.
Charlotte awoke this morning looking tired, and I asked her what was wrong. She was worried that her walking ability would continue to deteriorate, and that she would end up being paralyzed. Those thoughts are only natural to have, but I just hope her attitude continues to be one of her greatest assets.
She finished a sculpture last night, and just began another one this morning. I told her that says more right now than anything else.

December 31, 2009
Charlotte will start her Temodar tonight. Her UPC ratio is still too high for receiving Avastin. She has been having numbness in her right arm and leg. The numbness does not seem to be related to any loss of strength on her right side, which would indicate tumor progression. She does feel more comfortable walking with her mother's cane now.
She is scheduled for a cervical spine MRI along with her normal brain MRI on Jan 22nd.
Her last MRI was moved from Dec 28th to Dec 19th. It was read as "stable".

December 3, 2009
Charlotte will start her Temodar tonight, but she did not receive Avastin today. Her UPC (urine protein creatinine) ratio rose from 2.37 to 4.1 in the past week. On Monday, I convinced Dr. Spier to lower the Avastin dosage from 2.5 to 2.0 mg/kg and to raise the UPC ratio threshold from 2.4 to 2.5 in order for Charlotte to receive Avastin. My hope in changing these numbers was to keep her from missing an Avastin date.
The good news is that Charlotte read poetry last Saturday night at the Julian Christmas Tree Lighting Ceremony. It was cold with rain and snow (white dots in pictures), but she did a wonderful job. To attend and to read poetry was important to her, since it was two years ago at the same poetry reading that she started to slur her words.
Charlotte's brain seems to go through a "rebooting" two to three times a year now. When this happens, her speech becomes almost unintelligible. The good news is that she is aware something is wrong, and always says "what is wrong with me"? After a good night's sleep, her speech is back to "normal". This happened again on Tuesday, but I feel she has only regained about 80% of her speech. Her reading ability has also suffered about the same amount. She has also been "sick" for the past two days with a constant low grade headache and fatigue. If she gets any worse, I'll take her to the ER. She has always been good at letting me know when she needs to go to the ER. Most of the time she tells me "this too will pass with rest..."
Her labs yesterday were slightly improved over last week, except for her UPC ratio. I just e-mailed her nephrologist with an update on her blood pressure. I hope to increase one of her existing BP meds and try to stop her newest BP med (clonidine) that she has been taking for two weeks. I think the clonidine might be a big contributor to some of her latest symptoms.
Charlotte's Nov 24th MRI was read as stable. Clinical symptoms will probably be the first signs of tumor growth, especially when she is on Avastin. Clinical symptoms would be changes her speech, memory, walking, energy, etc. I think Charlotte's next MRI on Dec 28th will be very important to us.
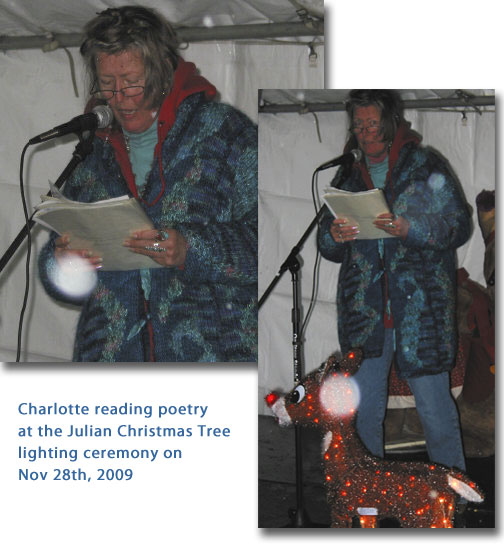
November 19, 2009
Charlotte had her Avastin today. Her labs yesterday showed both her platelets and her WBC count have rebounded. Her GFR (glomerular filtration rate) also rebounded from 57 to 86 in one week. Her chest cold and coughing have also slightly improved.
Her labs next Wednesday will be day 21 of her Temodar cycle, which means all of her blood counts will be at their nadir. That sometimes is not always the case, but it is something to keep in mind after receiving decent lab results this week.
Her next MRI is next Tuesday at 9:30pm. Hopefully I can get my disk copy sometime on Wednesday, just before Thanksgiving. There have been a few clinical changes in Charlotte since her last MRI, so I will be interested in what it shows. The lower dosage of Avastin (2.5mg/kg) seems to have kept the toxicity to Charlotte's kidneys at an acceptable level for now. I just don't know how well the tumor is being controlled at this lower dosage.
Nancy Grossmann (R.N.) and Kristine, both from oncology at Kaiser, attended Tom Oppenheimer's memorial service yesterday. Nancy said it was quite touching, and had brought back two pamphlets for everyone to see. I know Tom made a great impact on our lives, and from Nancy's description of his memorial, he had touched numerous other lives as well. We miss you Tom.
Nancy gave Charlotte a big hug as we left Avastin. She kindly held Tom's pamphlets behind her back as she hugged Charlotte since I had just told her that I had not informed Charlotte yet. Nancy's eyes began to swell as she hugged Charlotte. Not only have Charlotte and I been blessed to have known Tom and Mary for the past two years, but we have also been blessed to have had Nancy and her staff take care of us. There have been some very special people, both patients and staff, that we have met in the chemo room that have touched our lives. Thank you.

November 12, 2009
Just a short update on Charlotte, and then a tribute to our very dear friend Tom Oppenheimer.
Charlotte's labs yesterday contained both good and bad news. The good news is that her WBC count and platelets have risen since last week. The bad news is that her GFR (glomerular filtration rate) has fallen to 57, which is the lowest it has ever been. When her filtration rate fell below 60, she went from mild to moderate kidney damage. The other bad news is that she now has my chest cold that has been with me for three weeks. The chest cold manifests itself with uncontrollable coughing. The only good news is that she does not have a temperature.
Now to Tom and Mary Oppenheimer. Both Tom and Charlotte entered the Kaiser-UCLA trial study back in November of 2007. Their surgeries, radiation treatments, Temodar and Avastin treatments, MRIs, etc, were almost on identical dates. Some of our appointments with Dr Spier coincided, so we would have long talks and share information. They even went "off-study" within days of each other, Charlotte because of kidney toxicity due to the Avastin, and Tom's MRI showed he had tumor growth. At about the same time I was beginning to see what I thought to be tumor enhancement in Charlotte's MRI. Her PET scan on Sept 14th confirmed tumor growth, not in her old tumor bed, but in a different location.
Charlotte and Tom were the longest surviving participants in the Kaiser-UCLA trial study here in San Diego.
I just received an email from Mary Oppenheimer that Tom passed away on November 10th. He passed away quietly with Mary by his side.
God bless you both.
November 5, 2009
Charlotte had her Avastin and Temodar today. Her labs came back yesterday showing a UPC (urine protein to creatinine) ratio of 2.38. Dr Spier and I finally agreed that Charlotte could receive Avastin if her UPC ratio was 2.4 or lower. We also agreed that Charlotte would receive a new lower dosage of Avastin equal to 2.5 mg/kg. Her last Avastin was 5mg/kg. I'm trying to control the tumor while still keeping the toxicity to her kidneys low. All these numbers are arbitrary, so I have no idea what the results will be.
The labs also showed Charlotte's WBC count and platelets to be extremely low. In fact, my records show they haven't been this low for the past 20 months. That goes all the way back to March of 2008 when she was extremely sick due to the high dosage of Temodar at that time. These levels were a complete surprise to me, and obviously I am very concerned. Charlotte also woke up with a sore throat this morning.

October 28, 2009
I wanted to wait until Charlotte had her labs today before I wrote a short update.
The written MRI report by the neuroradiologist is not done yet, so the following are just my observations.
Charlotte's MRI on Monday looked "improved" to me. "Improved" means that her areas of enhancement did not look as bright, and in some cases, the enhanced areas were "almost gone". I say "improved" and "almost gone" because after hours of review, I just got the feeling that everything was still there, but was just being cloaked by the Avastin.
If the Avastin is ever stopped, I think everything will return.
I did find the new tumor that was first shown by the Sept 14th PET scan did in fact first appear on Charlotte's Aug 27th MRI. It appeared on that MRI as a very tiny white wisp, that then turned into a very small white dot on both her Sept 28th and her Oct 26th MRIs. That dot seems unaffected by the Avastin. I guess a more accurate statement would be that it's size has remained basically the same. It is located either in or next to her left hippocampus.
Charlotte has had more hypertension since restarting the Avastin, so it was not a surprise that her UPC (urine protein to creatinine) ratio had risen from 2.4 to 2.9 in just the last week. At some ratio, the Avastin will be stopped again. We have an appointment with Dr Spier on Monday, Nov 2nd. I want to discuss lowering the Avastin dosage even further. We need to find the correct dosage for Charlotte that will both control the tumor and spare her kidneys. There are so many variables that I can think of right now which could alter finding that correct dosage.
Clinically, Charlotte is doing fine. As I'm writing this, she's gluing the bails on more newly created fused glass pendants. She just finished a kiln shelf of Christmas decorations last weekend at the gallery. Hopefully I'll get those fired in the kiln sometime soon.
October 22, 2009
Charlotte had her Avastin today. Last Tuesday, we again drove up to the Kaiser complex on Sunset and Vermont in northern L.A. This time we had an appointment with Dr Michael Miller, another radiation oncologist. About 10 days before this meeting, I had received two emails from Dr Joseph Chen saying first that he agreed with Dr Spier that Charlotte should go back on Avastin, implying to me that radiosurgery was not an option. Later that same day, he wrote me again saying "I will have you and Charlotte come back to our radiosurgery clinic in Los Angeles so that we can discuss with my radiation colleagues. Will see you soon."
Dr Miller is Dr Chen's colleague, and basically that was how the consultation was conducted. We talked for an hour about Charlotte's MRI, SPECT and PET scans, what I thought were Charlotte's deficits (her short term memory and not being able to sometimes say the correct word), etc, etc. Dr Miller asked her about her artwork at the end of the meeting. For ten minutes Charlotte spoke flawlessly about Mary Oliver, Emily Dickinson and Walt Whitman, and how their poetry has influenced her sculptures. Go figure! Basically, the only thing that was definitely decided was just for everyone to wait until Charlotte's next MRI which will be this Monday, Oct 26th. Charlotte's BP at Avastin two weeks ago was 117/77. Today it was initially 151/101 before the Clonidine BP pill. Her UPC ratio has risen to 2.4, but her GFR (glomerular filtration rate) has gone from >89 to 64 (higher is normal). A level of 61 is the lowest it has ever been, and you don't want it to fall below 60. Again, all this has happened in only two weeks of being on Avastin.
I also have no idea what to expect on her next MRI. Obviously I don't want to see further enhancement, but if I do, maybe that could be pseudo-progression caused by the Avastin. The other extreme would be a scan that showed some decrease in the tumor, which one would think would be good. But Avastin can also "cloak" tumors, so I can not truly trust what the MRI is showing me. Obviously I would rather see a cleaner MRI than an enhancing one on Monday. That's why Charlotte's clinical status is so important to me. It tells me more, and sooner, exactly what the tumor is doing long before the MRI.
The picture below was taken by Donna today during Charlotte's Avastin.

October 8, 2009
Charlotte began her Temodar tonight.
We have had quite a few doctor meetings since the PET scan and the MRI. The MRI was read "abnormal" only because the same neuroradiologist had read the PET scan earlier and had seen the "hot spot", otherwise he said he probably would have read the MRI as "stable". The "hot spot" on the PET did coincide with a very small spot on the MRI which could have been easily missed.
To some of us though, the tumor that was located in the original site looked like it was starting to mobilize again. The tumor shown on the PET scan was more medial, and not located within the original tumor site. Our first option when the tumor grew again was to have surgery to remove the mass. We just never wanted to hear the two phrases: "it's location makes it inoperable", or "it's now a diffuse tumor".
Our first meeting last week was with a neurosurgeon who was willing to remove the new tumor revealed by the PET scan. We left his office feeling good, because our plan seemed to be on track. Surgery was an option, and we didn't hear the two phrases mentioned above. On Monday, we met with Dr Spier for the Temodar prescription, and she again suggested that Charlotte have fractionated radiation and to resume Avastin. These had been suggested to her by Dr Cloughesy at UCLA. Dr Pikul, our neurosurgeon in L.A., called me Wednesday after consulting with Dr Green, the neuro-oncologist in L.A. Dr Pikul told me that he would not perform the surgery because of the tumor's location, and that Charlotte needed a more "global" approach because the tumor was looking diffuse.
Today, we met with Dr Ijaz, a radiation oncologist, that performs IMRT radiation. He thought Charlotte's first choice should be to have radiosurgery performed by Dr Chen in L.A. That contradicted what Dr Chen had told us, and what Dr Spier had heard from Dr Cloughesy at UCLA. Charlotte was to restart Avastin tomorrow at 5mg/kg vs 10mg/kg. I cancelled that appointment because Avastin makes the brain more susceptible to bleeding if you have radiosurgery. I emailed Dr Spier to perhaps have a teleconference with Dr Ijaz, Dr Chen and Dr Cloughesy to try to get everyone on the same page regarding re-irradiation.
As Dr Ijaz pointed out today, we now have the following options:
1. Some type of re-irradiation, which I think none of the doctors want to do because of the possible side effects
2) Change/add a new chemo, which will be Avastin, which I don't want to do because of the possible side effects.
3) Do nothing.
The picture below was taken today a Tio Leo's with Charlotte's rosemaling on the booths. We did these booths 30 years ago.

September 24, 2009
I just received the written reports on Charlotte's PET and SPECT scans.
The SPECT scan was of low quality, but showed no definite or obvious abnormalities.
The PET scan showed a 7mm recurrent neoplasm.
I emailed Dr Pikul (awake craniotomy), Dr Chen (radiosurgery), and Dr Spier (neuro-oncology). Dr Pikul is out of his office until next week, so I will not have his opinion or suggestions until he returns. Dr Spier is also out of her office. I expressed my order of preferences to each of them. They are:
Surgery with Dr Pikul along with a biopsy and chemosensitivity testing from the tumor.
I don't know if 7mm of tumor will allow all of that testing.
Radiosurgery by Dr Joseph Chen.
Stronger chemo from Dr Spier.
Charlotte's next MRI is coming at a good time. It is scheduled for Monday, Sept. 28th.
September 10, 2009
Charlotte starts her Temodar tonight. Her lab tests yesterday showed her serum sodium was again at 137. Normal is 135-145. Her serum chloride had risen from 100 to 106 during the past week. Normal is 101-111, so that also looked good.
Charlotte is scheduled to have her PET scan on Monday, Sept 14th.
She will have the MRSpect on Thurs, Sept 17th.
Her 30 day MRI will be on Sept 28th.
All the above dates are still subject to Dr Pikul's approval.
September 4, 2009
Charlotte has had some busy days lately. On Sept 1st, she had labs done at Vandever. They had been ordered as a follow-up to her ER visit on Aug 27th, plus she had some normal chemo labs that were due. Later that day, we saw Dr Lin to discuss her labs, plus I had other questions about her kidneys and hypertension. All of her electrolytes were normal, and most of her other urine tests looked good, with a few exceptions. Dr Lin did not know why her serum sodium fell so much in just one week, and then recovered just as fast. He thinks her kidneys are in good shape, and that the Avastin is still causing her existing problems.
We saw Dr Joseph Chen Sept 3rd in northern L.A.
From Charlotte's notes, Dr Chen thought:
1. Radiosurgery may not provide the best results for a GBM.
2. He sees some enhancement, but doesn't know whether it is tumor or necrosis. He suggests that we request a PET scan and a MRSpect from Dr Spier.
3. Surgery by Dr Pikul will give us a sample for biopsy, which radiosurgery will not.
4. He thinks Charlotte's tumor is very slow growing as compared to a normal GBM.
5. He will do radiosurgery, but can not guarantee any long term benefits.
6. Necrosis may become more of a factor in this enhanced area after radiosurgery.
We saw Dr Spier on Sept 4th. She had sent me an email earlier in the week giving me a list of treatment options for Charlotte's enhancement. She also had called Dr Lai and Dr Cloughesy at UCLA to inquire about what we could add to Charlotte's Temodar. Dr Lai had done Charlotte's molecular testing. Both Dr Lai and Dr Cloughesy informed Dr Spier they thought Charlotte should go back on Avastin if we approved and if her nephrologist, Dr Lin, approved. They also said they would not recommend radiosurgery for Charlotte. Dr Spier also ordered the PET scan and the MRSpect that Dr Chen had suggested. She also ordered Charlotte's next MRI for the week of Sept 28.
Dr Pikul called me later that day and said he wanted the PET scan and MRSpect done and the results back by the end of next week. He was going to email Dr Spier to see if she personally could expedite these tests for him down here in San Diego. If not, Dr Pikul said he could order them done within a week up in L.A. Unfortunately, we would have to drive 250 miles for each test. I said "no problem".
The below picture is one that Charlotte walked two city blocks to have taken outside Kaiser at Sunset and Hollywood. It's for Donna!

August 27, 2009
I took Charlotte to the ER this morning. Over the past few days, she has been having increased mental confusion, an inability to speak correctly, nausea, fatigue and muscle weakness. She vomited at 4:30 this morning, and that was the determining factor. Her blood tests showed a serum sodium level of 122, normal being 135 to 145. A sodium level below 130 is known to cause all of the above symptoms, along with swelling in the brain. She was diagnosed with hyponatremia, and was given a sodium drip. She also had a temperature of 100.3 and high blood pressure. Charlotte was due for another MRI on August 31st, so they did the MRI today to rule out any tumor growth that might be effecting her speech. Dr Nordling read the MRI as stable. I talked with him while Charlotte was having the MRI and had expressed my concerns over certain views on the last two MRIs. I was able to get his written report later that day. He always writes the best MRI reports at Kaiser, but this one seemed to address some of my concerns. I will get my own disc copy tomorrow for comparison to the previous MRIs.
In the late afternoon, we were given the option by the attending ER physician, Dr Chen, to either take Charlotte home, or to keep her in the hospital overnight with an I.V. drip. Charlotte's nephrologist, Dr Lin, even came by the ER for a visit. Charlotte was eager to come home, but my concern was that I had read the only way to raise serum sodium was through a controlled sodium I.V. drip, especially in brain patients, and not through diet. Both Dr Chen and Dr Lin assured me that a diet higher in sodium would slowly raise Charlotte's serum sodium. We still don't know whether Charlotte's fever is being caused by an infection, or why her sodium level fell from 134 to 122 in just one week. She had only occasional vomiting during her last chemo, which is one of the main culprits of sodium loss. Dr Lin wants to see her next Tuesday for more tests. Dr Chen told me earlier that Charlotte's kidneys may not be able to hold in the sodium. Next Thursday we still have a consultation in northern L.A. for possible gamma knife surgery. That is going to be a long trip in Charlotte's condition. I think I'm beginning to see early signs of cachexia, so that will have to be discussed with her doctors.

August 13, 2009
Charlotte starts her Temodar tonight. Her MRI on August 3rd came back "stable". However, I have noticed some enhancement in her June 13th MRI and some further enhancement in her August 3rd MRI. We met with Dr Spier yesterday for Charlotte's Temodar prescription, and we went over the MRIs together. She agreed with me, and gave us a referral to see Dr Chen in northern L.A. He is in the same building as Dr Pikul, who said Charlotte would be a candidate for an awake craniotomy when the time comes. Dr Chen specializes in radiosurgery using the gamma knife. We see him on Sept. 3rd, and hopefully he will say that Charlotte is a good candidate. As Dr Spier pointed out yesterday, she wants to "nip this in the bud" before it gets out of hand.
The reason Charlotte's last two MRI's have been read as stable is that the enhancement that I see is mainly in only one view (saggital post gadolinium). Dr Spier said that before the neuroradiologist says "enhancement", they usually want to see it appear in two different views (e.g. saggital, axial and/or coronal).
I also just happened to read on the brain tumor research site yesterday about another GBM patient that thought she had seen some enhancement in her March MRI, but it too was read as stable. Her latest MRI shows the tumor has spread to the other side of her brain. She said that before a neuroradiologist says "enhancement", they must see reoccurrence at "above clinical levels", which she thought was enhancement of 24% or more. Yikes!
Charlotte's enhancement might be necrosis, scar tissue, or other things besides tumor growth, or some combination of the above.
Two good links:
Video of an awake craniotomy.
Meet Batman, a mixed breed german shepard with brain cancer.

July 16, 2009
Charlotte started her Temodar tonight. There have been both good and not so good clinical symptoms over the past month. The not so good have been her intolerance to both warm weather and especially the sun. She literally has to run from the sun. The good has been her appetite, and her ability to gain some weight. The small weight gain unfortunately has not transformed itself into muscle mass. She is still losing too much protein through her kidneys for that to happen. Clinical signs for GBM patients will probably present themselves long before a MRI picks up tumor growth. I judge her clinical condition by some obvious signs, and I think last week was one of her best weeks in a long time. Donna picked up on this change quite a few weeks ahead of me. Charlotte's alertness, reading, and speech have all been good. She even did her hair differently yesterday! Her physical activity, due to her muscle loss because of her kidneys, is probably my biggest concern now.
Most of the above is a good report, but that doesn't mean Charlotte won't be in the emergency room tomorrow. Nobody knows what change tomorrow, or next week, will bring.
In the last update I talked about visiting with Dr Pikul in L.A. for an awake craniotomy. I had to write myself another note and stick it to my computer to make sure that if she does have another surgery, that Dr Pikul sends the tumor off to Duke University for molecular testing and to Woodland Hills for chemosensitivity testing. This was scary to me because I have four three inch binders full of internet printouts, and I can not even remember some of these important facts. If the tumor is discarded, a lot of valuable information is lost.
Since tumor growth is so fast, as mentioned in my last update, one should also keep an up-to-date file on all family assets. Make sure all deeds and personal property titles show the correct owner names, etc. Charlotte and I may opt for an outside clinical study trial, and unfortunately Kaiser will not pay for any outside costs. We may have to get a loan ASAP to cover the costs, and having all the paperwork in one place is very important.
A quick note to all GBM patients needing financial help. Social Security passed "a compassionate disability act" (not sure of the wording) about a year ago for those people who have qualified for Social Security, but probably will not be around to collect it because of a life ending disease. It sounds good, and I recommend that every caregiver look into this program. Unfortunately, they have some weird "compassionate" rules, along with some very rude employees, so Charlotte did not qualify. I am a firm believer in "only positive thoughts" for cancer patients, and it was quite obvious how upset Charlotte was for days after this meeting. It was a big mistake on my part for putting her through this ordeal.
Charlotte's next MRI will be on Aug 3rd. Dr Pikul will initially read the MRI, since our neuro-oncologist will be on vacation until Aug 14th.

July 9, 2009
Charlotte and I went up to northern L.A. yesterday to see Dr. Pikul, who specializes in awake craniotomies. It was just a consultation about an option that Charlotte may have when her tumor returns. The visit started with Charlotte being given some speech and eye tests. We were very impressed with Dr Pikul, and I think he was impressed with Charlotte. He was great at going over Charlotte's last two MRI's with me, and listening to my concerns of what I had seen on her last MRI. He said it was appropriate to ask for her next MRI to be a week earlier. He does want me to call him on the day of Charlotte's next MRI. That statement by him was towards the end of the visit so I didn't get an explanation. He also kept emphasizing how important it was to get Charlotte back up to him for surgery as soon as possible when there is tumor growth. He said he has seen tumors double in size in just one week.
Charlotte is now off Avastin and officially off the UCLA study trial. She is presently just on Temodar. The other "star patient" of this study was enrolled at the same time as Charlotte back in Dec 2007. Mary Oppenheimer told me a few days ago that her husband Tom is now off-study due to tumor reoccurrence. Mary and I had a long talk about Tom and what to do next. She knows about my research. I told her that after all of my research, my hopes were that I would have a "Plan A or a Plan B" when we heard the words "the tumor has returned". I told her that unfortunately I didn't have those plans, and that I would probably follow whatever our neuro oncologist suggested. That is what Mary is doing with Tom.
My research has definitely increased my knowledge about this disease, and has changed my thinking about the various ways one might try to "control" this disease. But as I told Mary, both Charlotte and Tom went on and off the study trial at the same time, so who really knows the best treatment plan.
No one really knows who will be a long term survivor.
In the end, we can only do what we think is correct for our individual situation.

June 18, 2009
Charlotte started her Temodar tonight. Her Avastin is still being held because her UPC is still greater than 2.0. The UCLA study trial will only allow someone to be off Avastin for 90 days before they are dropped from the study. June 30th will be 90 days for Charlotte. I think Charlotte has clinically improved since being off Avastin, and her nephrologist is concerned about the long term effects that Avastin is having on her kidneys, so going off Avastin at this time is not so traumatic for us. Charlotte also had an MRI on June 13th. I have questions concerning some of the images, but I don't have the written report yet. The written report could change my mind about dropping Avastin.
Charlotte, Donna and I went to the Del Mar Fair today for 4 hours. Charlotte was, in Donna's words, just "awesome". She participated in an aerobics demonstration, had her picture taken with some show dogs, watched while Donna ate a cinnamon roll, and sat with me at the flower show. Charlotte did more in 4 hours at the Fair than she has done in the past year and a half!
Charlotte's energy medicine is named "Donna". There has always been a very special relationship between them for the past 40 years, and I have really observed it's effects every Thursday since Charlotte's journey began a year and a half ago. Every Thursday begins with the "normal Donna and Charlie", but by day's end, they both have enough vitality and exuberance to make it through the following week.
They are true soulmates!

May 21, 2009
Charlotte will begin her Temodar tonight. She came down with a "flu-like" viral infection on Monday, May 11th. She had a low grade temp, nausea, and most concerning, a low grade headache that was constant for seven days that even Tylenol would not relieve. The only food that she could handle was Ensure. On the sixth day, her fever finally went away, and she was able to eat some solid food. Her headache went away a few days later.
She obviously missed her chemo last week, so she is restarting her Temodar today. Her labs yesterday showed a UPC (urine protein creatinine) ratio of 2.1, and they will not restart Avastin until it is below 2.0. Her MRI came back stable and another test was not definative on telling us whether Charlotte's residual tumor
(what we actually see on the MRI) is actually tumor or radiation necrosis. I was hoping for that information, so without it, she will probably be restarting Avastin when the trial study allows it. Charlotte and I have some deep concerns about restarting Avastin.
The echocardiogram results showed some enlargement of Charlotte's heart. Just like the proteinuria, the Avastin increased her BP to the point that it was damaging both her kidneys and heart. We do have her BP under control for now, but only due to some very powerful BP meds that have their own side effects.
Right now, it is a toss up whether I'm more worried about the tumor, or the side effects of the chemo, radiation, and all of her other meds.
Brain cancer link.
I have Charlotte enrolled in the Virtual Trials case history and treatment section.
It's a good basic site to begin your journey.

April 30, 2009
Charlotte did not have her Avastin today. Sorry for my confusing update last time. When she does resume the Avastin, it will be at the lower dosage of 5 mg/kg. The Avastin will be held until Charlotte's urine protein creatinine ratio is less than 2.
Her urine protein creatinine ratio did fall from 8 to 6.8. At least we are heading in the right direction. I'm still getting some very high BP readings, but I'm also getting some normal readings too. Charlotte had an EKG yesterday and the cardiologist said the abnormalities were probably due to her high BP. She will have an echocardiogram tomorrow.
She will also have her MRI next week. I have noticed some clinical changes in her, so the MRI is coming at a good time. Hopefully these changes are not from the tumor, and being off of Avastin, but are from her radiation treatments, BP and proteinuria problems, etc.
I have received a lot off feedback concerning my links to other GBM information.
The first one is about MRI imaging analysis of GBM patients which contained nice images. Too technical for most, but was one of the best links that I have found.
This second link is just a touching story.

April 16, 2009
Charlotte will have her Temodar tonight, but we were notified yesterday that Avastin will be held due to the level of protein in her urine. I don't know if we will be able to continue with the UCLA Avastin and Temodar study trial. I did officially ask them to lower the Avastin dosage to 5 mg/kg from 10 mg/kg. The UCLA regulatory board is evaluating my request, but I am not optimistic for their approval.
Charlotte did see a nephrologist last week. Even with changes in her BP meds, her urine protein creatinine ratio jumped from 1.7 to almost 8.0 in the past two weeks. Her renal and BP problems have made her very tired. There are other other side effects that I am not happy seeing. We saw Charlotte's neuro-oncologist, Dr. Spier, last Monday. She was great about saying "O.K." to all of my requests.
While writing this update, I just learned that UCLA did approve the 5 mg dosage of Avastin. The following are two emails I just wrote, instead of rewriting this update:-
Hello Dr. Spier,
I just sent this to Nancy.
Even though we would not lose you if we went off study, sometimes doctors are not thanked often enough by their patients. I appreciate your help during the teleconference with UCLA.
Thank you for everything!
Hi Nancy,
What a surprise about the 5 mg dose of Avastin!
I had a massive headache yesterday, plus a feeling that things were starting to slip in a direction that I did not want. I have had a love/hate relationship with Avastin for the past three months, but that really was not my fear yesterday. My biggest fear was that if we did go off study, we would lose you.
I don't think you know how much we are truly grateful for you, and the work you do for us.
Thank you,
Brent and Charlotte

April 2, 2009
Charlotte had her Avastin today. Her lab tests yesterday showed her UPC (urine protein creatinine) ratio had risen to 2.9, up from 1.7 two weeks ago. The study trial will hold the Avastin treatments when the ratio reaches 3.5, so today was probably her last Avastin for a while. I have asked to see a cardiologist and a nephrologist ASAP. I hope these specialists will have more knowledge about Avastin, and the effects it has on BP and proteinuria. Charlotte's BP is out of control, and this was an avoidable situation.
I want to thank Nancy Grossmann (R.N.) at Zion Kaiser, and her study trial staff, for all of their conscientious and professional help.

March 19, 2009
Charlotte had her 14th cycle of Avastin and Temodar today. Her UPC (urine protein creatinine) ratio has risen from about 1.1 to 1.7 in the last two weeks due to the Avastin. Her last MRI results came back "stable" again.
We had a wonderful visit with her brother Gary and his wife Lorie last weekend. The picture below shows all of us on the sofa in the gallery.
Last week my update included information on Avastin. This week it is mainly about Temodar. Again, these are random lines from random posts from random people taken during the past two weeks. I thought these would be of interest to those of you that are fighting this terrible disease. (Thank you to all the authors.)
--------------------------------------------------------------------------------------------------------------------
Something else to worry about: "Temozolomide, a standard treatment for brain cancer, may boost the aggressiveness of surviving cancer cells, making tumor recurrence more likely, a new study suggests." This study is from Memorial Sloan-Kettering Cancer Center.
Re: Temodar promotes bad stem cells? Here's the link to the full paper
"Clinically, what we see with patients with glioblastoma is that after surgery, radiation and chemotherapy with temozolomide, they live longer and a subset of them will actually live a year, two years or even longer. And then pretty much 100 percent of the patients relapse and no one knows why."
"When you treat mice with temozolomide they develop recurrent diseases even quicker, so temozolomide make the cells that survive act in a more aggressive manner." "Temozolomide actually increased the number of drug-resistant cells. Because temozolomide doesn't target ABCG2, it may render surviving cells more resistant to treatments that do target the ABCG2 protein."
A paper presented at the last ASCO conference (google: asco 2008 Quant) concluded that once Avastin has failed that there is little benefit in trying other agents in combination with Avastin...
I also don't know if cediranib has been tried after Avastin but, personally, I think that's a reasonable idea, since it's an anti-angiogenic with a somewhat different mechanism than Avastin. I think that combining cediranib with lomustine (CCNU) also makes sense, since CCNU is a cytotoxic agent, although the toxicity always needs to be considered. "A safe bet: cediranib will be most effective with CCNU."
It's been a busy month for news already! In tomorrow's issue of the JCO (Journal of Clinical Oncology), an update on a study I've been following for 3 years will appear with very encouraging results. The regimen is essentially standard GBM therapy with an added dose of CCNU (lomustine) once a month. The results compared to standard therapy are remarkable. The new update in tomorrow's JCO. Moreover, I think this regimen could be a top choice for any newly diagnosed grade IV patient who does not get into a Novocure or vaccine trial, especially those outside the U.S. with a methylated MGMT promoter gene.
As another TMZ option for recurrent GBM, go to p863 at link to download Strik et al's full paper. One recent study that produced data re diffuse recurrence was Naranya et al.
Conclusions: Antiangiogenic therapy using bevacizumab appears to improve survival in patients with recurrent high-grade glioma. A possible change in the invasiveness of the tumor following therapy is worrisome and must be closely monitored.
This may be a rather simplistic explanation but here goes: my husband has no progression around the original tumor area. Instead he has what has been termed a delicate invasive spread of the tumor cells in a quite large area- they barely even show on the MRI. These cells do not depend on making blood vessels the way that the GBMs usually do. Instead these cells live off of pre-existing blood vessels. They have taken different pathways that the Avastin is not blocking as they have mutated or learned to escape the stronghold that Avastin used to starve them. I don't think the Avastin "drives" the invasiveness. It's just what happens as the tumor cells find their way around the Avastin.
There are a number of angiogenesis compounds that can be secreted by cells when under distress due to shortage of oxygen and nutrients. Avastin targets only one of them: VEGF-A. My understanding is that if the cell is not 'satisfied' with the results of emitting VEGF-A, then nature has programmed the cell to begin to release other angiogenesis agents (I think there may be as many as 10 that have been identified). These other 'second-line' signaling agents may be giving the tumor a different growth pattern.
I agree that Avastin is very scary, but when faced with inoperable tumors, and if failure on TMZ happens, other than vaccine trials what options are out there?
"A new 600-page book entitled "Integrative Oncology" just came out, and I highly recommend it:"

March 5, 2009
Charlotte had her Avastin today. On Tuesday, her teeth were cleaned by her friend Grace Hansen. The picture below shows the two of them before the cleaning.
I would like to thank our friend Leena Hannonen for updating our website. She is presenting a series of mosaic workshops in Julian. Please visit her website. You can see all of the information at artelitedesigns.com
Charlotte's labs continue to show the effects of the Avastin on her body. There has been mention of Avastin (bevacizumab) on some of the brain tumor sites with some linked studies. Below are just random lines from random posts from random people during the past week. This is obviously not my usual update, but I thought this change was important. (Thank you to all the authors.)
................................................................................................................................................
We tried several other options but avastin was the only thing that was successful - even if only for 6 months. It gave him a chance to spend quality time with our children and grandchildren and to celebrate one more
Christmas.
So my bottom line is that I hope patients still consider using Avastin, but keep the emerging pitfalls in mind, and explore dosing schedules, combination therapies, and potential prophylactic treatments which maximize
the benefits while limiting the side-effects.
He likes to remind patients that "everything works in mice, but you are a human".
He is hugely full of hope, and truly believes we face chronic diseases, not terminal ones, and treats accordingly.
I don't think the article should be viewed as a universal condemnation of such therapies or Avastin in particular.
Patients should recognize both the known strengths and weaknesses of Avastin at the time of decision-making and avoid blanket statements which limit their options.
One of the general principles of cancer biology is that if one growth path is blocked, the cancer will try to find another path. In the specific situation of Avastin failing, we're in uncharted territory. However, given cancer biology, I would suggest going after 2 or more other growth factors, using something like Tarceva or a new multi kinase inhibitor. This is just a guess, however, in an area we clearly need suggestions!
This kind of aggressive treatment strategy may best be obtained from Duke, in keeping with what I understand is their reputation. You now need to move beyond using NIH as consultant.
The tumor is like a diffuse cloud.
Diffuse tumors tend to co-opt existing vessels rather than spawn new ones. That could be how the tumor is surviving - Avastin won't kill off normal existing vessels. Has anyone on these lists been able to effectively control their tumor once it has escaped the Avastin stronghold? If so how long has it been and what
have you used?
My son is in the same spot--he has failed Avastin. The tumor is spreading diffusely around, affecting his sight and speech. He is in a bad spot.
This news release in Science Daily addresses "angiogenesis inhibitors— succeeds at first, but then promotes more invasive cancer growth". Nothing new, for those of us who have been tracking the bevacizumab
story.
Has anyone on these lists been able to effectively control their tumor once it has escaped the Avastin stronghold? If so how long has it been and what have you used?
High vascularization of glioblastoma typically predicts poor prognosis.
Neovascularization (vasculogenesis and angiogenesis) is essential for tumor growth and invasion.
Vascular endothelial growth factor (VEGF) is a critical proangiogenic factor in almost all solid tumors. However, its expression and role in human carcinoid development and progression remain unclear.
The sometimes controversial cancer drug Avastin can cause kidney damage by doing what it's supposed to — but in the wrong place, a study shows. Edema is generally associated with tumor progression. Avastin has a half-life of about 20 days, and CPT-11 is less than a day, so if it's been longer than 20 days, your husband is officially off treatment.
These data indicate that stem cell-like tumor cells can be a crucial source of key angiogenic factors in cancers and that targeting pro-angiogenic factors from stem cell-like tumor populations may be critical for patient therapy. My understanding is that the cancer stem cell hypothesis is still under investigation and debate.
How bad is that? Well his tumor suddenly looks like a diffuse ghost spreading up through the frontal lobe and also crossing over a little into the other side of his brain. It's amazing that his scans were absolutely clean last time and now it's sort of everywhere. If it helps, Barbara, mine is in, and crossed the corpus, and is slightly into the right side, all that area is diffuse (not the lump seen elsewhere)
Are they absolutely sure that it is tumor? I assume that the changes that they are seeing on the MRI are on the T2 FLAIR images. But T2 FLAIR enhancement can also be from radiation/treatment related effect too. It can sometimes be very difficult to distinguish between the two on MRI images alone. If they are seeing mass effect, then tumor is likely.
He has been on avastin/temodar treatment and suddenly developed extensive FLAIR enhancement surrounding the right frontal tumor cavity, crossing the corpus callosum to the other side. It was very scary looking on the scan. The differential diagnosis at that time was radiation related change versus infiltrating tumor. He had no
symptoms. There was also no mass effect on the MRI. We went for a Dopamine PET scan at UCLA which was cold, so it was decided that the changes were not tumor after all.
The use of various contrast agents in MR imaging is becoming a challenging field of neuroradiology research. Iron oxide nanoparticles shorten T1 and T2 relaxation times, so they can be used in MR imaging of malignant brain tumors...
You have been quite an inspiration to all of us. May God be with you and my prayers are there for your fast and successful recovery.
Just because it is back again, does not mean it's going to win!!! The GBM has already tried to get me in 2000, 2004, and 2007 and never got the best of me! Now in 2009 I am going to beat the battle again. I'm ready for the
challenge.
Yes, blood glucose levels do make a big difference, both in prevention and treatment of most cancers (if not all). This is why so many researchers are interested in ketogenic diets, the IDH1/IDH2 genes, and other aspects of glucose metabolism.
I am so sad to read this - yet another challenge for you all to face. Diffuse tumors are so hard to measure. Maybe this can explain some of the clinical symptoms he has been having.
Also, here's a paper on aerobic glycolysis...
How to get the wacky stem cells under control!
O.K., I exhausted everything you have up that I hadn't already read.
Here's a decent article in Newsweek which I just stumbled across. It overviews cancer research, and largely echoes the findings of a previous article in Fortune by Clifton Leaf. www.newsweek.com
Here's a mini-lesson in chemo drug metabolizing. You can generally look up the metabolism of any drug by Googling the drug's scientific name and the words "metabolism" or "pharmacokinetics."
....All of these potentially cause drug interactions through interference with a key metabolizing enzyme called CYP3A4, part of the main family of metabolizing enzymes called cytochrome P450 (abbreviated "CYP").
.....Temozolomide (TMZ) is a prodrug, meaning that it is inactive by itself and only takes on its therapeutic qualities when it is metabolized. TMZ is hydrolyzed at physiologic pH to the active compound, MTIC,
without the aid of metabolizing enzymes. TMZ is essentially 100% bioavailable.
You might create some sample (food) menus of what a high grade brain tumor (patient) might take.
If metronomic TMZ has failed at 50 mg/m2, I'd be reluctant to try it at 75 mg/m2 because you would add toxicity and might not add to efficacy, though I could certainly be wrong.
Unlike P53 or PTEN mutations, IDH mutations only cause glioma but not any other cancers. Why it is so specific is with no doubt under intense investigation in academics. For us as patients, I care about how to make use of the findings in my treatment.... My first thought was IF (a big if) the loss-of-function mutation causes accumulation of isocitrate and a deficiency of alpha-ketoglutarate, and IF (another big if) alpha-ketoglutarate-deficiency indeed drives tumor progression, supplementing glioma patients with alpha-ketoglutarate may do the trick. This sounds like a crazy idea. It can not be this simple, can it?
Fatigue and balance issues are common in GBM for many reasons ranging from chemo to radiation to seizure medications to tumor progression. It's very difficult to pinpoint the cause.
I'm glad we have an international group here!
Malignant gliomas are highly lethal cancers that depend on angiogenesis for malignant progression
The base of pneumocytis pneumonia is a yeast, in the candida family. Steroids and antibiotic and temodar all can aide and abet this fungus. Candida in many forms is a HUGE issue for cancer patients, especially with meds and treatments and steroids.
I also recommend checking out the lively panel discussion on molecular oncology which can be found here.
Ultimately, your doctor is not responsible for your treatment and health. You are. Nobody is going to care more, or have a bigger vested interest in your survival, than you. And sometimes that means you have to think outside the box, and seek out evidence-based treatments on your own.
Thank God you guys are dedicated toward fighting this monster!
The following article explains the Avastin kidney damage (proteinuria) issue.
I just got my last MRI at UCSF last Friday. At that time I was told "It all looks good -the same and clear, no seen tumor". I drove home happy. Today I got a phone call from my Neuro-oncologist at UCSF.....
With Peace, Love and Hope...
God Bless...
Tons of love to you...
Wishing you strength....

February 19, 2009
Charlotte had her Avastin and will start her Temodar tonight. Lab tests show that her white blood cell count remains low, and Avastin is still making her kidneys produce protein in her urine. Another side effect of the Avastin is to cause her to have hypertension. Her blood pressure seems to have stabilized over the past few weeks, so we have not had to immediately go back on a third B.P. medication. Her sodium and chloride are still a tad below normal since she was discharged from the hospital.
We have had some inclement weather during the past two weeks, so instead of going for walks, she has been going up and down our back stairs. It is definitely more of an aerobic exercise than walking, and works a different set of muscles in her legs. It works her heart a lot more than just walking, which I like.
For the past couple of weeks, she just seems more tired than usual. Plus I think she has lost another four pounds, which does not make me happy. But I know her drugs are cytotoxic, and are influencing the tone of her muscles.
There are a lot of the doctors and nurses out with the flu, so I am trying to protect Charlotte from getting sick. She was out with me this past weekend trying to get fallen trees cut up. Over my objections, she told me that we have always worked together as a team, and this was no different. I finally convinced her to throw the ball for the dogs, in between supervising me.

February 5, 2009
Charlotte had her Avastin today and then we had our usual "get together" lunch with Donna and friends.
Charlotte's lab yesterday showed that her blood sodium level was still slightly low and her potassium level slightly high. These electrolyte levels are about the same since she was released from the hospital about ten days ago. Her neuro-oncologist pointed out that giving Charlotte "salt tablets", which she has been given in the past, could be dangerous. Raising the sodium level too fast in a brain patient could do more harm than good. I filed that away somewhere in my head because Charlotte has different doctors that prescribe medications for her different conditions. Comments and statements either get a little red flag (meaning I do not totally agree) next to them in my head, or a check mark (meaning it could be good upon further research). A little red flag went up about two weeks before Charlotte was admitted to the hospital on Jan 18th, and I blame myself for not looking into matters further.
The attending physician in the ER did make a comment about Charlotte's nausea and vomiting during her chemotherapy, and her statement received a little check mark. After confirming her statement, I decided to give it a try. Charlotte started her twelfth Temodar and Avastin cycle on January 22nd. It was the first time in a year that she did not have any chemo related nausea and vomiting. That allowed us to walk, work, etc., during this normally bad time of the month. We will see if next month produces the same results.
Looking back over the past year, there were two major things that made me feel so helpless. One was the sound of her vomiting during chemotherapy. That is why the above paragragh is such good news for us. The other was when I had to inject her with Neupogen to stimulate her bone marrow. The shots were given for three consecutive days, and she had to have them twice during the past year. The big side effect of the shots was to make her bones very achy. Waking up in the middle of the night hearing your wife moan and cry just to turn over in bed is something I will never forget.
On a happier note, Charlotte has expressed interest in writing a book about her brain tumor journey. She feels she has a lot to offer to her fellow comrades, especially with breast and brain cancer. I do not know the logistics of doing something like this, but I do think it would be a truly remarkable book.
I vividly remember going out and buying Dr. Susan Love's "Breast Cancer Book" with Charlotte right after her breast cancer diagnosis in 2001. We took turns reading it aloud to each other while trying to determine the best course of action.
Today, the type of cancer is obviously different, but the techniques remain the same for me. Learn as much about this disease as possible. Unfortunately, there is not one definitive book like Dr. Love's that we can go buy on brain cancer. Thank goodness for all the scientific sites like PubMed on the internet. There are a lot of things that I have learned that I wish I would have known a year ago, and those would be my contribution to Charlotte's book. Treatments are always changing, but one must know where to go to at least begin. I did not even know this in the beginning. I would like to pass this knowledge on to others.
I truly believe that with a glioblastome multiforme brain tumor, you only get one window of time to control this type of cancer. Obviously my job, along with others, is to learn how to keep that window open.

January 22, 2009
Charlotte started her Avastin and Temodar today.
Charlotte had a low grade nausea for most of last week and was accompanied by some vomiting as the week progressed. Charlotte's blood pressure also increased dramatically Friday night, and then her brain temporarily misfired. She had a somewhat similar condition right after brain surgery while staying in the hospital in December 2007. I asked her my name, her date of birth, and the names of our dogs. She could not say them, but unlike a year ago, she knew that she was unable to speak the correct words. She kept saying, "What is wrong with me, why won't the words come out?" She became very frightened. This "word to mouth" pathway has become noticeably more difficult for her. Realizing this, and knowing that I thought she did know all the names but just could not say them, I gave her a pen and paper on which to write. She proceeded to write the correct answers to all of my questions. I told her not to worry, it is just a matter of some physical therapy to retrain certain pathways in her brain. I do not know what caused this incident, but the positive is that she kept communicating to me that she knew what was happening to her. A wonderful book given to me by Mary is "My Stroke Of Insight" by Dr Jill Bolte Taylor: A Brain Scientist's Personal Journey. Charlotte's episode could have been an addendum to her book.
Then on Sunday morning she awoke with a headache, which meant an immediate trip to the emergency room at Kaiser. She was diagnosed with having a very low sodium level due to her vomiting and to a diuretic that she had recently been prescribed for both her BP and her kidneys. She was also diagnosed with a bladder infection. Charlotte was hospitalized after our ER visit, and on Monday she had a brain MRI to rule out any tumor growth or edema. Her MRI came back stable, so she was discharged late Monday, which helped us keep her next appointment at 8:30am on Tuesday with her neuro-oncologist. We also had an appointment today after the Avastin with her primary care physician to evaluate her blood pressure and her proteinuria, but was cancelled by his office early this morning. It will be rescheduled when he returns to his office.
Yesterday, after going to the lab for more tests and then off to pick up a copy of her latest MRI, she was able to put the finishing touches on a sculpture, dance with me in the kitchen to a Billy Joel song, and hug and kiss me about eighteen times.
What a beautiful and inspirational woman!
I am the luckiest man in the world....and I know it.

January 8, 2009
Charlotte had her Avastin today. Yesterday's lab work showed she had an increased level of protein in her urine. That is the third weekly lab that showed an increase. Right now we are just watching the level and hoping it does not get worse. Proteinuria describes a condition in which urine contains an abnormal amount of protien. Avastin can cause proteinuria, which can progress into kidney failure. Proteinuria has been associated with cardiovascular disease. High blood pressure can also cause proteinuria. Avastin also contributes to her high blood pressure.
It seems like it is a vicious circle, trying to control the tumor while still keeping the rest of her body healthy.
I remember reading some articles written by professional caregivers. The gist was more patients eventually succumbed to the side effects of their treatments than from their cancer. I do not know if that is true, but I still try to remember that everyday. It is so easy to live from one "stable" MRI to the next, and to forget about the rest of the body.
We are back walking twice a day, which is so important to her overall health. The rainy weather had reduced the number of walks for a period of time. I think her stamina is as good as it has ever been during the past year. Most importantly, she looks and feels great. Her ability to find the correct word when she speaks remains her biggest problem.
The wonderful pleaure she has is to wish her sister Donna a very, very
!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!Happy Birthday!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!!

December 26, 2008
Charlotte's MRI on Dec. 15th came back "stable". She started her Avastin and Temodar today.
This has been one of the hardest months for her after her last Avastin and Temodar. She started with more nausea and vomiting, and her "chemo fog" has been with her for most of the time. Problems with her short term memory and her ability to find the correct words when speaking, seemed to have all slightly increased. All of this does not worry me at this time. We actually start laughing at her new language. She usually knows her wording is incorrect before I realize it. We will see how she does this coming month. I have read about patients receiving "stable" MRIs but also have clinical deterioration while on Avastin. That is something that would concern me, but her overall appearance and actions are still very good. Plus she can still play her flute and read out loud perfectly. Her artwork is getting more exquisite!
Last week I received a copy of all of Charlotte's MRIs on a disk. There were a total of ten MRIs dating back to November 26, 2007. I am trying to compare all of the MRIs to each other, and then compare each MRI to each written report. I have found a few good sites on the internet concerning how to interpret MRIs of GBM patients. My first big learning experience has come from comparing each of Charlotte's MRIs. I do not know the meaning of what appears on the MRI, but I can say that her brain has not been static during the past year. I asked a doctor if some of these "white wispy clouds" (axial T-2 FLAIR) meant more tumor, ischemic problems, brain softening, edema, or effects of treatments. This is something that I will try and learn myself, or through my long list of contacts.
I would like to thank Dr. Lai and Dr. Cloughesy at UCLA, and Dr. Polikoff, Dr. Spier, Dr. Silbert and Dr. Nordling at Kaiser in San Diego. I especially want to thank my brain researcher friends "Hong" and John Williams for helping me interpret some of Charlotte's tests. John, your wealth of knowledge is truly over-whelming, and your kindness in sharing is enormously appreciated. Your understanding and awareness of seemingly every GBM scientific abstract, both in vivo and in vitro, and the time that you must spend doing this research and then answering your emails from people like me, is just astonishing!
Finally, thank you Nancy Grossmann(RN) and your staff at Kaiser.

December 11, 2008
Charlotte had her Avastin this afternoon. The past two weeks have been very busy and sometimes confusing for us. First, we had Charlotte's teeth cleaned by our very dear friend, Grace Hanson. She reminds me so much of Charlotte. She is very competent, intelligent, and has that certain beauty both inside and out.
Charlotte's Avastin and Temodar just seemed to be a lot harder on her this month.
That has also been reflected in some of her blood counts. Some months seem overly good, such that I can not really trust them, and then some months they drop to a new low. Her blood pressure was extremely high again this morning. That has always been a constant battle.
Our philosophy, from both our personal experience and the experiences of others, is that you just have to take one day at a time. And as a caregiver, you must be aware conditions can change very fast. I am still haunted by the line from a friend's email that stated "I wish I would have done more for him". That is something that I never want to feel. Charlotte is on a cancer diet that may or may not be effective, and that is also why I had her teeth cleaned. Sadly these were never discussed in the beginning. But eating right, and trying to stop secondary infections from entering her body through her gums just seems to be the correct decision for us.
I still spend hours reading as many scientific abstracts that my mind can "comprehend" each day and night. Actually, when I first started one year ago, it was like reading a foreign language. I spent more time looking up and then writing down the definitions of these words. About two months ago, I sort of had an epiphany. I realized things were sort of making sense to me for the first time.
Emphasize "sort of"! I now have a new respect for all medical professionals and researchers, and all of their training. They are also in a field that brings forth new knowledge everyday. I personally can not understand how one individual can be fully informed in each of their specialties.
I want to mention that Charlotte had heart palpitations and vomiting last Sunday at 3AM. She had an EKG on Wednesday, but we have not received the results. Charlotte's next MRI is scheduled for Monday, December 15th. Those following five days are becoming more and more stressful for me. It usually takes about a week to get the results if the tumor is stable. But our neuro-oncologist will personally call us during those days if new growth should appear. I know the facts, and know our chances of avoiding that phone call lessen with time.
Charlotte's next Avastin and Temador will start December 26th.
We want to wish everyone a Merry Christmas, and a "thank you" for your love and prayers during the past year. Everyone has been so kind and generous that I do not know where to begin. I will not even try, except to say that I know that each and everyone of you have helped Charlotte fight her battle. And for that, I am truly humble.
Merry Christmas. Be well everyone. Love, Charlotte and Brent

November 30th, 2008
Charlotte had her Avastin on Friday, and we started her Temodar that night. She was suffering from a bad headache that was brought on by the Avastin for all of Friday. She told me late Friday that she felt that it would probably be best if we did not go up to Julian. For her to say that seemed very unusual to me. As I mentioned in the last update, it was one year ago at the Julian Christmas Tree lighting ceremony that she read some poetry. That is when we knew something was wrong. On Saturday morning she felt better, and decided that she wanted everyone to see and hear her reading poetry again.
She did a beautiful and inspiring reading of three poems on Saturday night! Unfortunately we had to return to San Diego early Sunday due to the side effects of the Temodar. We want to thank the wonderful Julian Library for inviting her to participate again.
Also, a very special "thank you" to Leena Hannonen of ArtElite (www.artelitedesigns.com) for designing our website and for posting our updates over the past year. Her expertise and friendship has made this past year endlessly more helpful and comforting for Charlotte and me. Thank you Leena for your many hours of work that you have generously given to us.
From Leena: It's been my plasure
to be able to do this for you and I treasure your friendship.
November 18, 2008
Charlotte had her Avastin last Thursday, and will have her next Avastin and Temodar on Friday, November 28th, the day after Thanksgiving. Hopefully she will be able to attend the Julian Christmas Tree lighting ceremony the day afterwards, on Saturday November 29th. It will mark her "one year anniversary". It was at last year's tree lighting that she also read some poetry, and she started to have slurred speech. The next day she was diagnosed at Kaiser as having a brain tumor.
The attached five photos are a record of our progress over the past year. Obviously the first photo was taken before her diagnoses. The following photos show her at different times as she progressed during the year, ending with a photo that was taken just a few weeks ago. It's been quite a journey. One cancer researcher that comes to the gallery told me that many cancer patients have to reach their nadir before they seemingly get better. I would like to look at the pictures with that in mind. But, then days like yesterday happen. Charlotte woke up with a severe headache and was vomiting. That was very unusual. Always thinking of the worst first, I thought of possible bleeding in the brain from the Avastin. After watching her closely, and talking with her during the day, it turned out to be just another bump in the road that we've come to live with in the past year.
I've been busy trying to learn as much as possible about Glioblastoma Multiforme. Currently, I've been reading Charlotte's MRI reports from the past year and trying to educate myself on the terminology in the reports. Her latest MRI show that she has "chronic ischemic (inadequate supply of blood) small vessel disease" and a "contrast enhancing mass associated with postoperative encephalomalacia (softening of brain tissue by vascular changes). Then there is the residual tumor with "slight rim enhancement".

Every night I read more scientific abstracts on numerous GBM topics. It is over whelming, and sometimes quite discouraging, but I've always believed that knowledge is power. There is a whole world of information out there, from cancer diet to cancer therapies, that caregivers must research and learn.
One example is Ben Williams (teaches at UCSD) who was diagnosed with glioblastoma in 1995. The following is from his website.
“Treatment for GBMs and other high-grade gliomas is changing rapidly. Until the last five years there was a standard treatment in the USA , including surgery, radiation, and chemotherapy with a nitrosourea, either BCNU alone or CCNU combined with procarbazine and vincristine (known as the PCV combination). While this treatment has worked for a small minority of people, its 5-year survival rate has been only 2-5%. Alternatives to this traditional treatment regimen are imperative if GBM patients are to have any realistic hope of surviving their disease. Fortunately, new treatments are now being introduced at a rapid rate. But unfortunately, most still are not available outside of clinical trials and there is no consensus about what is the best treatment for this deadly disease.
"There are two general premises to the approach to treatment that will be described. The first of these is borrowed from the treatment approach that has evolved in the treatment of AIDS. Both HIV and cancer involve biological entities that mutate at high rates. This implies that unless a treatment is immediately effective the dynamics of evolution will create new forms that are resistant to whatever the treatment may be. However, if several different treatments are used simultaneously (instead of sequentially, which is typically the case), any given mutation has a much smaller chance of being successful.
"A second general principle is that any successful treatment will need to be systemic in nature because it is impossible to identify all of the extensions of the tumor into normal tissue. Moreover, cancer cells are typically evident in locations in the brain distant from the main tumor, indicating that metastases within the brain can occur, although the great majority of tumor recurrences are within or proximal to the original tumor site. Localized treatments such as radiosurgery may be beneficial in terms of buying time, but they are unlikely to provide a cure. Even if the localized treatment eradicates 99.9% of the tumor, the small amount of residual tumor will expand geometrically and soon will cause significant clinical problems.
"Until recently, the only systemic treatment available has been chemotherapy, which historically has been ineffective except for a small percentage of patients. An important issue, therefore, is whether chemotherapy can be made to work substantially better than it typically does. Also becoming available are new systemic treatments that are much less toxic than traditional chemotherapy. The availability of these treatments raises the possibility that some combination of these new agents can be packaged that is substantially less toxic and yet provides effective treatment based on several different independent principles. Thus, the AIDS-type of combination approach is now a genuine possibility whereas it would not have been ten years ago. Because oncologists have been slow to appreciate the significance of the increased availability of these relatively nontoxic treatments, patients learn about them piecemeal if at all. Thus, patients themselves need to become familiar with these new agents and the evidence available regarding their clinical effectiveness. It is possible, although by no means proven, that some combination of these new agents offers the best possibility for survival.
"Patients may or may not learn about the treatments that will be described from their physicians. To appreciate why this may be, it is important to understand how American medicine has been institutionalized. For most medical problems there is an accepted standard of what is the best available treatment. Ideally this is based on phase III clinical trials. Treatments that have been studied only in nonrandomized phase II trials will rarely be offered as a treatment option, even if the accepted "best available treatment" is generally ineffective. What happens instead is that patients are encouraged to participate in clinical trials. The problem with this approach is that most medical centers offer few options for an individual patient. Thus, even though a given trial for a new treatment may seem very promising, patients can participate only if that trial is offered by their medical facility. An even more serious problem is that clinical trials with new treatment agents almost always study that agent in isolation, usually with patients with recurrent tumors who have the worst prognoses. For newly diagnosed patients this is at best a last resort. What is needed instead is access to the most promising new treatments, in the optimum combinations, at the time of initial diagnosis.
"Physicians rarely will inform a patient about clinical trials being conducted elsewhere. Moreover, the idea that several different agents from separate phase II clinical trials might be combined will be met with great resistance. Patients themselves will therefore need to become informed about what options are available, and which kinds of combinations seem most promising. In addition to the information that will be presented here, other information, especially about which new clinical trials are available, are available elsewhere on this website (address: www.virtualtrials.com ).”
October 30, 2008
Charlotte had her Avastin this morning and will start her Temodar tonight. We will be trying to attend our "Julian Open Studio and Gallery Tour" at our gallery this weekend. Hopefully the nausea caused by the Temodar will be kinder to her this weekend so that she can enjoy her friends. Charlotte right now has a slight headache from the Avastin, but is in very good spirits. We actually have a few people to thank for that.
First, her sister Donna, for always being there at the Avastin treatments, and then bringing laughs and smiles to our faces during lunch. Lunch was at Tio Leo's again today, and thank you again Pete for making it so enjoyable.
And a very special thanks again to Nancy Grossmann, R.N., at Kaiser Permanente for putting up with my never ending questions while Charlotte is getting her Avastin. I can not say enough about how much she means to us.
Another thank you to Dr. Iris Lowe for doing her chiropractic work so that Charlotte is able to continue to walk, and even work, without her being in pain. Walking is so important for patients that are on Avastin to avoid blood clots. One gallery Charlotte wants to visit again is Gallery 21 in Spanish Village in Balboa Park. First, she has so many friends in Spanish Village that she would love to visit again. Dr. Lowe is also currently in a show "Friends of the Chinese Brush" now at Gallery 21 (October 30 -November 17) from 11-4pm . Unfortunately we will not be able to attend the reception this Sunday (4-6pm). But seeing the show and all of her friends in Spanish Village will fit nicely into one of our "walking routines".
Finally, the news about Charlotte's last brain MRI was that her tumor is "stable".

October 20, 2008
Charlotte had her Avastin last Thursday (Oct.16th). We had another appointment with Charlotte's chiropractor, Dr. Iris Lowe, that same evening to help Charlotte with some hip, shoulder and neck problems. Dr. Lowe felt Charlotte's upper vertebra were starting to fuse together, which kept her from walking in an upright position. She came out of there looking, and most importantly, feeling like a new woman.
Charlotte and I worked together at the gallery over the weekend because Mary had a beautiful wedding to put on for a dear friend. It was good to see Charlotte interact with all of the customers, and then find time to work on a small sculpture. Charlotte had a 7am appointment at Kaiser on Monday (Oct, 20th) for her bimonthly MRI. I think there have been some policy changes at Kaiser because now they make you wait about a week for the "official" MRI report if everything is stable. They do a cursory look within 24-48 hours to see if something abnormal appears, and will let you know. But for some reason, as we were leaving because our 20 minutes were up with our neuro-oncologist, I believe she happened to mention that she no longer reads the MRI ahead of time. It's too bad because I think she is, in my opinion, the most qualified to read the MRI. She has seen things that the regular neuro-radiologist has not seen. We fully trust and respect her. I get the feeling that Kaiser is starting to demand some policy changes from their doctors that are not necessarily in the patient's best interest, but I could be wrong. Anyway, I guess we are now in the routine of "no news is good news" for the week. Which, for a proactive husband with a wife with brain cancer, is troubling. I receive emails from other patients and they asked me about this new delay in finding out about their MRI. I told them just what I said above, but that I didn't question it during the visit. I know the clock is running during our appointment, so I told them that I always prioritize my questions before entering.
I must mention, the one true angel since day one, when no other doctors or nurses were around to respond to my urgent emails, etc., is Nancy Grossmann, RN, at Kaiser (Zion). She is the liaison nurse between the study trials and the patients in oncology. She has always returned my phone calls or emails, and helped us in so many ways. Kaiser, give her a pay raise, but don't give her any vacation time! I panic when I know she is not there!
My main job for the last three months has been trying to weigh our options for when Charlotte's tumor returns. As previously mentioned, usually the tumor comes back with a vengeance, and is usually no longer responsive to chemo drugs. Also the Avastin may cloak the tumor so that the MRI looks great, but the clinical condition of the patient declines. Avastin may also make the tumor come back in a more diffuse pattern, so surgery may not be an option. These are just a few of the things that have come out concerning Avastin. I think for Charlotte her best option would try to get into a vaccine trial at UCLA. I've emailed Dr Linda Liau who is charge of the program. The big restriction (besides the cost) is that Dr Liau would need to do another resection on Charlotte for a fresh tumor sample in order to make the vaccine. Due to UCLA's policy and regulations, this surgery can only be done at UCLA, not Kaiser. Our neuro-oncologist thought that the trial could cost us $100,000. Another option for us would be If Charlotte's tumor comes back as an operable mass that could be resected at Kaiser, I could then send the tissue sample to the Weisenthal Cancer Group in Huntington Beach for tumor cell profiling. They would test Charlotte's cancer cells against 20-30 chemo drugs (and combinations) to see which might be most effective. But again that's chemo, and after Avastin, chemo may not be effective. Plus, I've seen it first hand, the body can take only so much chemo. I think the vaccine would be a lot easier for her. Another limiting factor for Charlotte is that most trials want newly diagnosed GBM patients. Charlotte will now be classified as a patient with a recurrent GBM. That limits my options for finding a trial study even further. I don't even know if Charlotte would qualify for the above vaccine trial. There are so many limiting factors to consider (trial cost, trial location, Charlotte's health at the time of reoccurrence, etc.). I just hope Kaiser will give me answers to my questions in a timely manner so that I can further decide what options are actually viable for us.

Charlotte working on "Hope"
October 2, 2008
Charlotte had her Avastin and Temodar today. She had to have a special blood pressure medication (Clonidine) just before the Avastin because her blood pressure was too high. Generally, this has been a month with problems for her, but yesterday she looked magnificent to me. Her normal blood pressure medicine has been increased, and a new blood pressure medicine has been added. She seemed to have her "chemo fog " for all of the month instead of just a week following the Temodar. Her speech and memory have just slightly regressed. But she reads her Mary Oliver, Sarah Teasdale and Walt Whitman poetry out loud every night, along with playing her flute. To me, all of these are inspiring and well done. And of course her sculptures are exquisite. I even had her help me with some Internal Revenue Service forms and some California State Board of Equalization forms. It was sort of a test, since the "math" side of her brain was where most of the GBM (glioblastoma multiforme) was located. She still managed to do a good job.
I have learned you can not just ask her questions in order to find out exactly how she is doing. Some things are obvious, but usually I have to be more intuitive. I remember when she came out of surgery at Kaiser Permanente, the nurse was testing her and asked her who the President of the United States was. She couldn't say "President Bush", but she answered that she could draw his face for the nurse. Today, if she met either Senator Obama or Senator McCain, she would shake their hands, complement them both equally, and tell them each to have a wonderful day. She does that to everyone now. I think that is what aggressive cancer brings out in the truly special people of this world. She has this very strong belief that every person is precious, and needs to be acknowledged. She has always felt this way, but these feelings seem to grow in intensity with each passing day.

Charlotte working on a sculpture last week.
See the archives here.

Please come back to this page for updates on Charlotte's new journey.

Charlotte Mitchell - Poetry In Glass
The love of words inspires artist Charlotte Mitchell to create sculptures
mostly out of her favorite material - glass; a wonderfully, colorful medium.
However, she augments glass with many other materials such as new ceramics
and metal and precious, recycled fire fragments; filling the creations with
strength and beauty - inside and out.
Charlotte loves poetry, which has caused her to create her art. She has
created beautiful works based on the imagery which fills her mind when reading
poetry, song lyrics or other words-well-done. Her inspirations may take her
to another part of the world or another time in history. One of the first
poems that inspired such works was the last line of "The Summer Day" by
Mary Oliver, an unfamiliar poet’s work which Charlotte found taped
near the front of a friend’s computer —"Tell me, what do
you plan to do with your one wild and precious life..." The imagery
of Mary Oliver’s poetry has sent Charlotte’s mind to the forests
of Massachusetts, and has lead her straight to Tibet. Mary Oliver is now
one of Charlotte’s favorite poets. Walt Whitman’s powerful words
has led Charlotte onto the Sea, or onto the Grass. Many sculptures are related
to old-time hymn lyrics such as "Amazing Grace", or "old-seeming" lyrics
by Sting - "Fields of Gold". All of these go directly to the hearts
of people who enjoy beauty or who can regain joy from visions of both the
words and sculptures.
One of the largest pieces is called "Something There Is" from
Robert Frost’s "Mending Wall". Fire-flashed glass, metal,
ceramic faces , and recycled oddments frame a seven-foot wall which wants
to crack open as the glass swirls up and out the top of the wall. Built after
the 2003 Cedar Fire, this piece has made a tremendous impact on viewers.
Charlotte Mitchell finds the showing of her artwork at the Julian Library
both a honor and a privilege. She hopes to show what words and art can do
to our lives.
See the archives here.
Visit The Mitchell Studio Gallery
4336 Highway 78 (at Wynola Rd), Julian,
CA
760-765-1102
Hours will depend on her health, so please call ahead.
It is a bright yellow 110 year-old building
with lots of flare, love, and
grace!
Enjoy!
See more photos from the gallery here.
 |
![]()













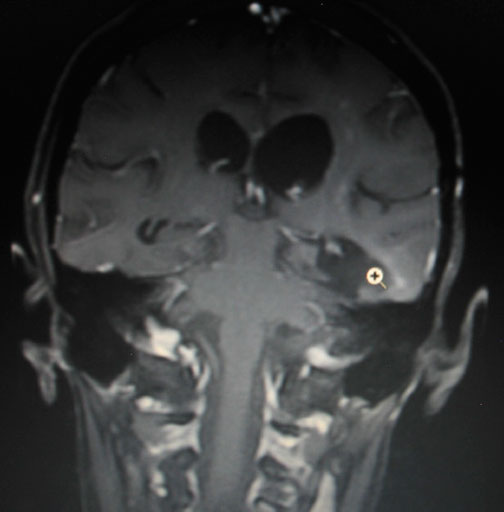
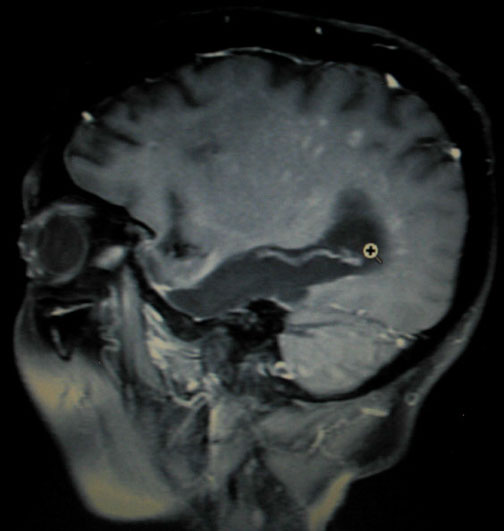


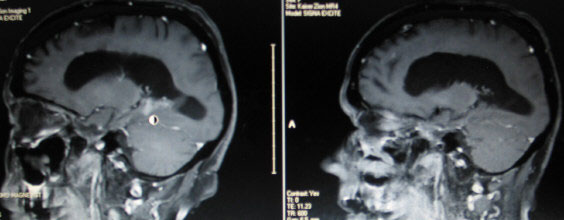
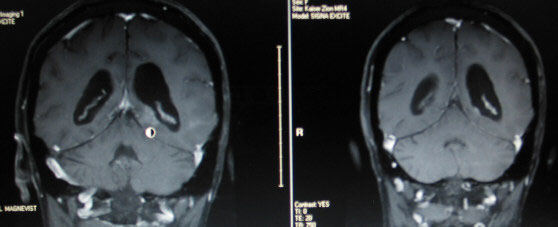
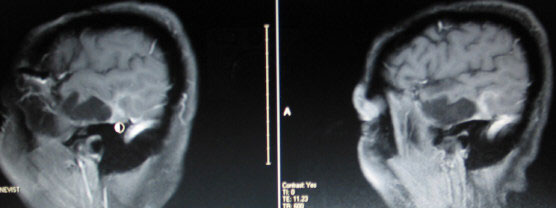

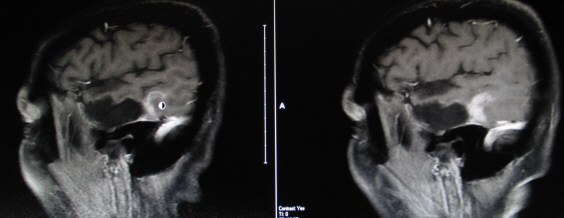 image 2
image 2
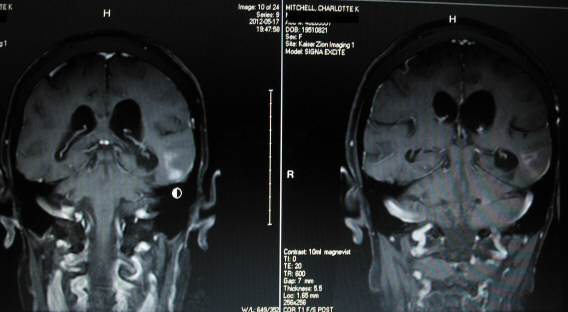
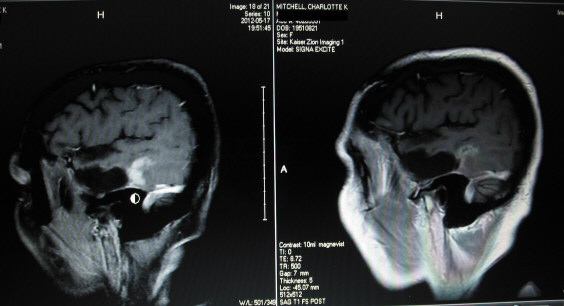





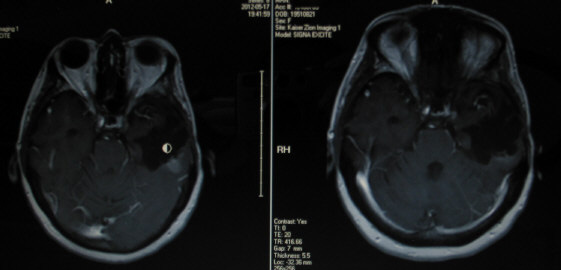
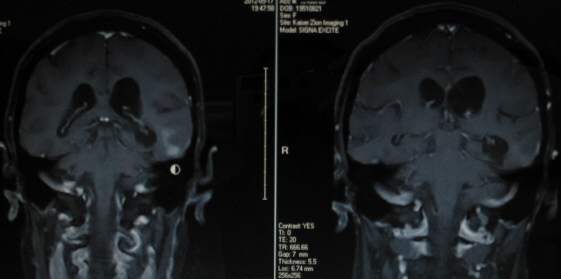
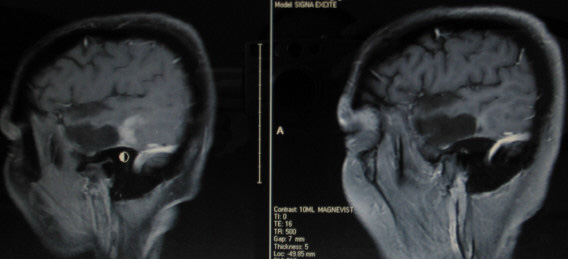


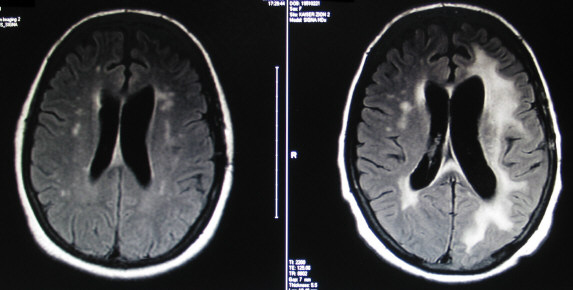
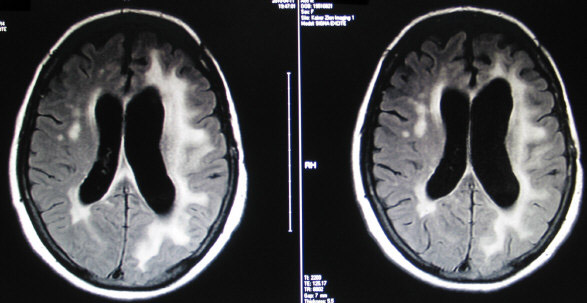
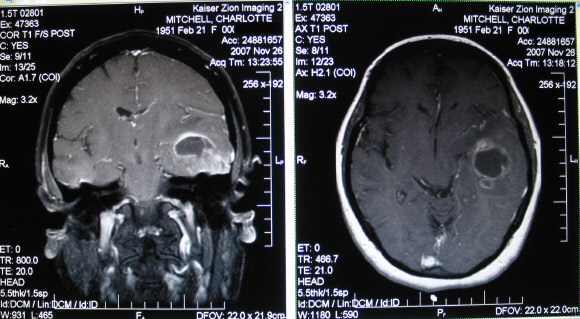

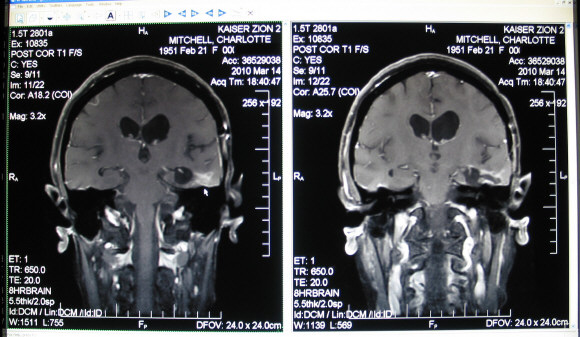
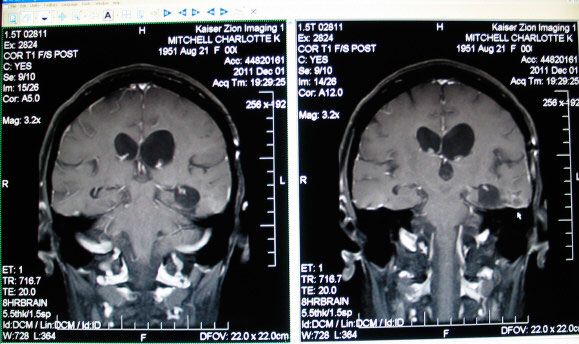


































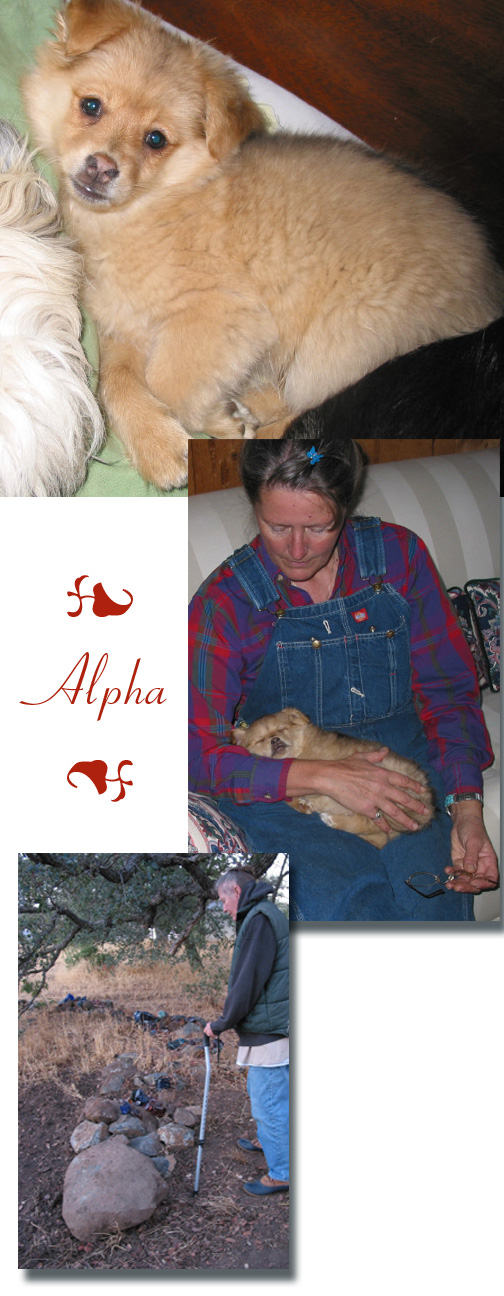
 .
.